Surgery, Gastroenterology and Oncology

|
|
Introduction: Synchronous esophageal and lung cancer is an uncommon entity with few descriptions in the literature. It poses a relevant challenge to health care providers regarding its management and surgical approach.
Case report: We present the case of a 73-year-old male diagnosed with lung squamous-cell carcinoma after admission for a history of productive cough and episodic hemoptysis. An esophageal squamous-cell carcinoma was diagnosed. Both tumors were histologically different. A surgical procedure was conducted with concomitant esophagectomy and lobectomy. The patient had no postoperative complications and was discharged home after 15 days post-surgery.
Conclusions: The diagnosis of synchronous tumors is challenging and should be based on clinical, imaging and histological criteria. Choosing to perform a surgical procedure for resection of both tumors in the same operative time represents a technical challenge, but has shown to have good impact on morbidity and mortality. Documenting such cases is important in order to improve management of these clinical situations, allowing for better outcomes for these patients.
INTRODUCTION
Synchronous malignancies are defined as two or more primary histologically distinct malignant tumors occurring in the same individual, not representing an extension, recurrence or metastasis and whose diagnosis is made within a 6 month time span (1).
Esophageal and lung cancers represent two of the most fatal malignancies worldwide, with low survival rates (2). The coexistence of these malignancies is an infrequent clinical entity, with few cases described in the literature. It is imperative to perform na adequate staging, when two distinct masses in these locations are found, as it has an important impact on the therapeutic strategy and overall prognosis of these patients (2-4).
The best approach should always be multidisciplinary and decided case-by-case due to its specificities. Combined surgical resection of esophageal and lung tumors is a feasible and safe option, with good outcomes in terms of morbidity and mortality. However, it represents a technical challenge, with potential hazardous post-operative complications (4,5).
CASE REPORT
A 73-year-old man presented to the Emergency Room with a 1-month history of productive cough and episodic hemoptysis associated with chest pain.
DISCUSSION
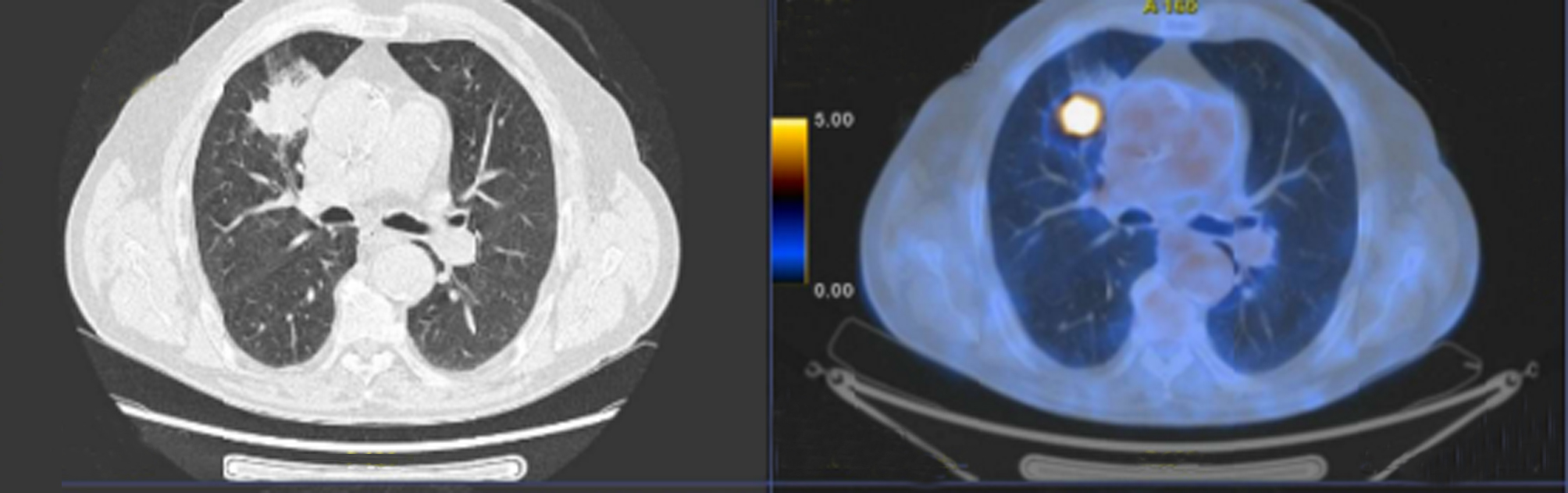
The patient was admitted, and further investigation was performed. In a chest computed tomography scan (CT-scan), a nodular, gas-filled lesion with wall thickening in the anterior segment of the right upper lobe was found. Later, a broncoscopy was performed and the diagnosis of squamous-cell carcinoma was made. Further along the investigation, a positron emission tomography–computed tomography (PET-CT) was performed, showing a hypermetabolic focus in the middle third of the esophagus. An upper endoscopy was performed revealing a vegetant ulcerated lesion at 25cm from the incisor teeth (figs. 1 and 2). Biopsies were performed and a squamous-cell carcinoma was diagnosed. CT-scan of the neck, abdomen and pelvis showed no further suspicious lesions, with no signs of metastatic disease. According to the TNM staging system, the esophageal tumor was a T1-2N0M0 and the lung tumor was a T3N0M0.
Figure 1 - PET scan image of esophageal lesion

Figure 2 - PET scan image of pulmonary lesion.
The case was discussed in multidisciplinary meetings both in the Esophagogastric Surgery and Thoracic Surgery department and the decision was to perform a thoracoscopic right upper lobectomy and a minimally invasive McKeown esophagectomy.
After successful anaesthesia with two cavity endotracheal intubation, patient was put in a left lateral
position and right upper lobectomy via vídeo-assisted thoracoscopy was performed, followed by thoracic oesophageal mobilization and lymphadenectomy via thoracoscopy. Next, patient was turned to a supine position and abdominal laparoscopy was performed. Upper abdominal lymphadenectomy was done, followed by stomach mobilization and construction of the gastric conduit (Akiyama tube). Cervical approach was done through a cervical left lateral incision, esophagus and gastric conduit were sectioned, and surgical specimen removed. A mechanical latero-lateral esophagogastric anastomosis was constructed.
The lenght of the postoperative stay was 15 days, with no postoperative complications. The final histopathological examination revealed a basaloid squamous-cell carcinoma of the esophagus with no positive lymph nodes (pT1b N0 R0) and a low differentiated basaloid squamous-cell carcinoma of the lung, also with no positive nodes, but with venous invasion and invasion of the pleural inner lamina (pT2b N0 R0).
Case was rediscussed in multidisiciplinary meetings and patients was proposed for adjuvant chemotherapy for the lung cancer. A surveillance follow-up strategy was proposed for the esophageal cancer.
CONCLUSION
Since the first reports of synchronous malignancies in 1889, more case reports have been published in the literature (4). This entity poses various challenges in terms of diagnosis and management strategy. Multidisciplinary teams and experienced surgeons in high-volume centres are essential to treat these patients successfully.
In our case, both tumors had a similar histologic type, which difficults in establishing if we are dealing with two different tumors or rather a primary tumor with metastatic disease on a second location. Establishing this distinction should be based on clinical, imaging and histological criteria. Therefore, tumor staging and preoperative evaluation is of utmost importance and should be very thorough.
Multidisciplinary approach and multimodal therapy may include surgery and (neo)adjuvant treatment with chemoradiation therapy. Decision regarding the best treatment option for each patient must account for patient’s functional status and comorbidities (6).
The definition of the therapeutic approach comprises a number of options, such as surgery, chemotherapy or radiotherapy, which must take into consideration the patient and consequent morbidity (6).
In our case, surgical procedures for lung and esophageal resection are highly complex and associated with potential morbidity with a high risk of postoperative complications, especially in elderly patients and in those with important comorbidities with limited functional capacity and previous pulmonary disease (3).
Minimally invasive surgical approaches are associated with fewer post-operative complications, are ontologically safe and may be a valuable option in these cases.
Overall, case reports of synchronous esophageal and lung cancers are scarce in the literature. Also, due to its rarity, reporting such cases is of great importance as it highlights the multidisciplinary approach and discussion regarding diagnostic and management strategies, helping improve surgical outcomes and disease prognosis, with a potential impact in patients’ survival and quality of life.
Author’s contributions
All authors have been actively involved in the reported case and take full responsibility for the
content of this article.
Conflict of interests
All authors state no conflicts of interest.
Ethical statement
Written informed consent was obtained from the patient of this case report.
REFERENCES
1.Soerjomataram I, Coebergh JW. Epidemiology of multiple primary cancers. Methods Mol Biol. 2009;471:85-105.
2.Zhao H, Misariu AM, Ramirez-GarciaLuna JL, Nobel T, Mueller C, Cools-Lartigue J, et al. Synchronous Esophageal and Lung Cancers-Is Combined Anatomic Resection Appropriate? Ann Thorac Surg. 2022;113(4):1354-60.
3.Mukerji AN, Wolf A. Synchronous Esophageal and Lung Cancer. Thorac Surg Clin. 2018;28(1):97-104.
4.Li X, Fu J, Zhang H, Zhai Z, Wang W. Synchronous carcinoma of oesophageal and lung treated with laparoscopic-thoracoscopic cooperative surgery: A case report. J Minim Access Surg. 2020; 16(2):169-71.
5.Buyukkarabacak Y, Pirzirenli MG, Gurz S, et al. Treatment options for synchronous lung and esophagus tumors: A difficult decision to make. Turk Gogus Kalp Damar Cerrahisi Derg. 2023;31(1):136-42.
6.Ishii H, Sato H, Tsubosa Y, Kondo H. Treatment of double carcinoma of the esophagus and lung. Gen Thorac Cardiovasc Surg. 2008;56(3):126-30.
Full Text Sources:
Abstract:
Views: 370

For Authors
Journal Subscriptions

Mar 2024
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
 IASGO Society News
IASGO Society News