Surgery, Gastroenterology and Oncology
|
|
ABSTRACT
Background: Congenital intestinal malrotation is a rare developmental anomaly due to incomplete rotation and fixation of the midgut during fetal life. Though predominantly identified in infancy, it can exceptionally present in adulthood, often with nonspecific symptoms that pose a significant diagnostic challenge. This case report discusses an adult presentation of intestinal malrotation complicated by volvulus, with successful surgical management. A comprehensive review of the literature is also provided, highlighting the embryological development, clinical spectrum, diagnostic modalities, and current therapeutic strategies.
Case Presentation: A 20-year-old male presented with a three days history of vomiting, diffuse abdominal pain, and obstipation. Physical examination revealed abdominal distension and tenderness without peritoneal signs. Contrast-enhanced computed tomography revealed a markedly distended cecum and the 'whirlpool sign' indicative of intestinal volvulus. Emergency laparotomy confirmed the diagnosis and ileocecal resection with anisoperistaltic ileocolic anastomosis was performed. Postoperative recovery was uneventful.
Conclusion: Adult intestinal malrotation, although rare, represents a potentially life-threatening condition. Clinical awareness, appropriate imaging modalities and timely surgical intervention are critical to minimizing morbidity and mortality. In adults presenting with unexplained abdominal symptoms, a high index of suspicion is warranted. Early recognition and prompt operative management remain key determinants for favorable outcomes.
INTRODUCTION
Intestinal malrotation is a congenital disorder resulting from an aberrant embryological development of the midgut. During normal embryogenesis, the midgut undergoes a complex sequence of elongation, herniation, rotation, and fixation between the 5th and 12th weeks of gestation. This includes a 270-degree counterclockwise rotation around the axis of the superior mesenteric artery (SMA), positioning the small intestine predominantly on the left and the colon on the right. Failure in this rotation or fixation process may lead to malrotation, characterized by abnormal bowel positioning, a narrow mesenteric base, and predisposition to volvulus (1,2).
Although this condition typically manifests within the first year of life, adult presentations — either acute or chronic — are well documented but rare, accounting for only 0.2–0.5% of all intestinal obstructions (3). The presentation is often protean, ranging from asymptomatic cases discovered incidentally to life-threatening acute bowel obstruction or ischemia.
Embryological Development and Intestinal Rotation Mechanism
The embryological development of the gastrointestinal tract involves three key stages:
• Stage I (5–10 weeks): Physiological herniation of the midgut into the umbilical cord, with a 90-degree counterclockwise rotation;
• Stage II (10 weeks): Return of the midgut to the abdominal cavity with an additional 180-degree rotation;
• Stage III (11 weeks to term): Fixation of the intestines in their final anatomical positions, with the duodenojejunal junction placed to the left of the midline and the cecum in the right lower quadrant (4).
Disruption at any point in this sequence may result in distinct forms of malrotation, each with anatomical and clinical implications:
• Non-rotation: Characterized by a failure of the midgut to complete its normal 270° counterclockwise rotation. This results in the small intestine being predominantly located on the right side of the abdomen, with the colon abnormally positioned on the left;
• Incomplete rotation: Occurs when the duodenojejunal (DJ) junction fails to reach its proper position in the left upper quadrant. This is often associated with peritoneal (Ladd’s) bands
crossing over and compressing the duodenum, leading to partial obstruction;
• Reverse rotation: Represents a rare variant in which the midgut rotates in a clockwise direction, positioning the colon posterior to the superior mesenteric artery (SMA) and potentially causing vascular compression or obstruction;
• Segmental malrotation: Involves rotational anomalies confined to a specific segment of the intestine, such as the jejunum or ileum, leading to atypical presentations and challenging diagnoses (5).
All of these variants share a common anatomical consequence — a narrowed mesenteric root — which significantly increases the risk for midgut volvulus, internal herniation and duodenal obstruction. Recognition of these patterns is crucial, as their complications may present acutely and require urgent surgical intervention.
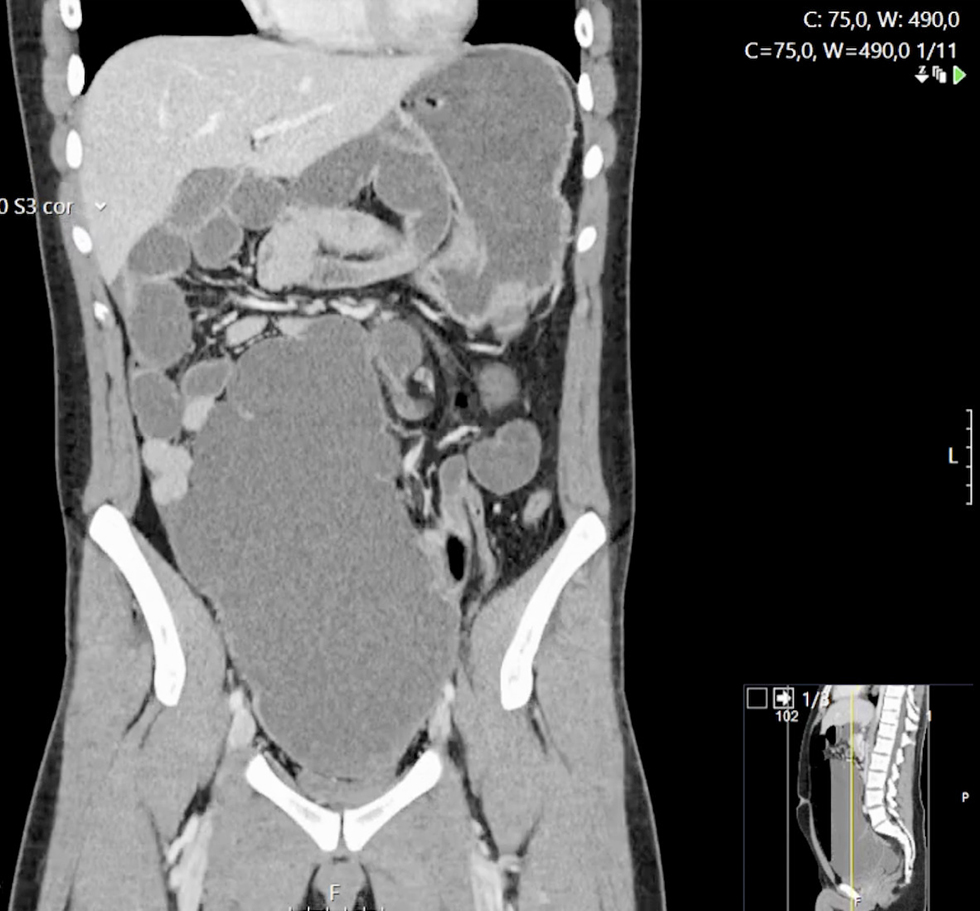
Figure 1 - Coronal CT image showing significant cecal distension and the ‘whirlpool sign’ due to twisted mesenteric vessels, suggestive of midgut volvulus.
CASE REPORT
A 20-year-old male with no significant medical or surgical history presented to the emergency department with a three-day history of vomiting, generalized abdominal discomfort, and absolute
constipation. He denied fever, weight loss, prior similar episodes and other symptoms.
On examination, he was afebrile, hemodynamically stable, but appeared in distress. The abdomen was distended and tympanic with diffuse tenderness, but with no rebound or guarding.
Laboratory findings included normal values for hemoglobin (16.4 g/dL), mildly elevated leukocytes and C- reactive protein (11000/mm³ and CRP 12.73 mg/L, respectively), with normal renal function.
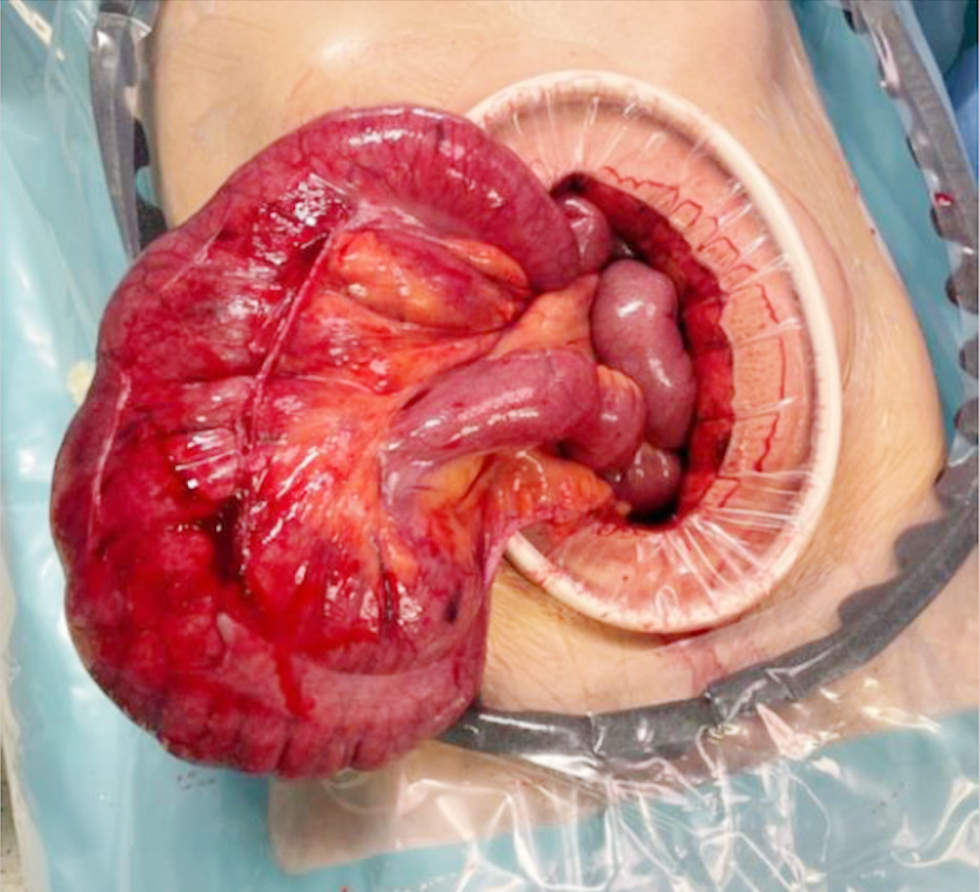
Figure 2 - Intraoperative view demonstrating markedly distended cecum without ischemia or perforation.

Abdominal radiographs showed multiple air-fluid levels. Contrast-enhanced computed tomography (CT) of the abdomen and pelvis revealed marked cecal distension (13.5 cm), whirlpool sign indicating twisted mesenteric vessels and a malpositioned duodenojejunal junction and small bowel loops (fig. 1).
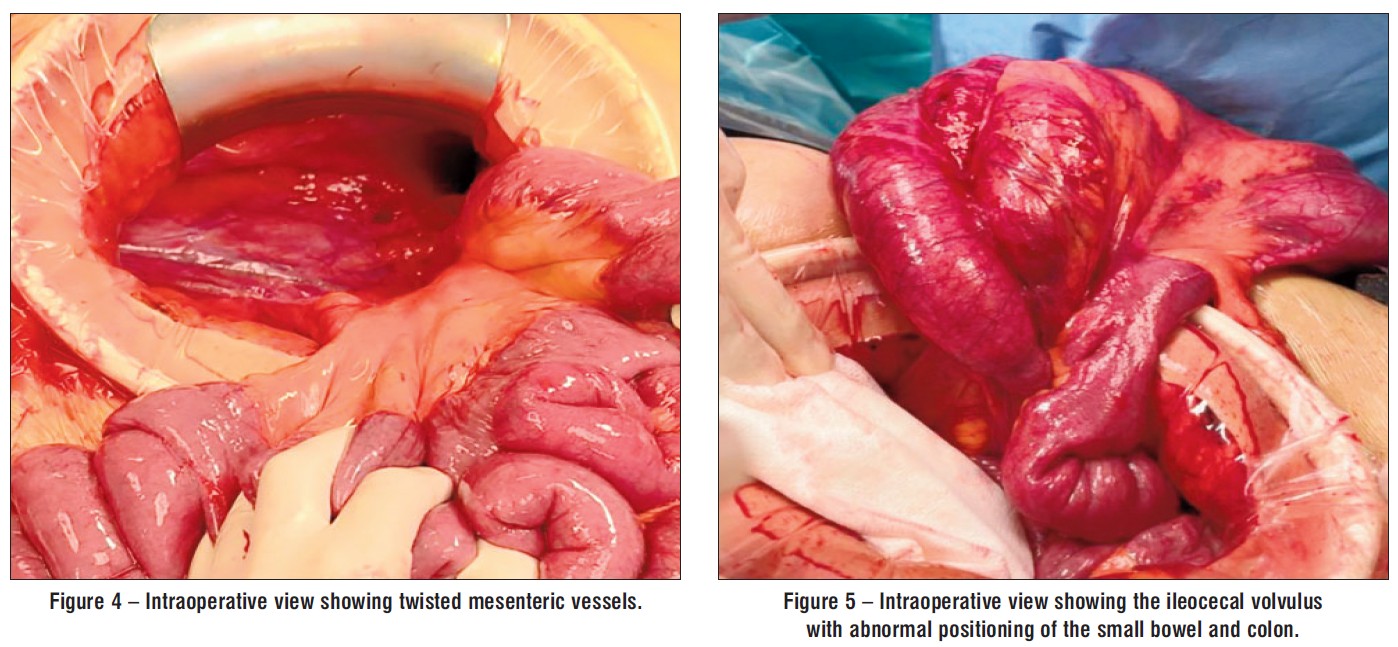
Due to the marked distension of bowel loops, the surgical team opted not to attempt a laparoscopic approach. He was instead submitted to emergency laparotomy. Intra-operatively it was evident the presence of the small bowel entirely on the right side, colon entirely on the left and a tight volvulus of the ileocecal junction with no ischemia or perforation (figs. 2-5). A modified Ladd's procedure was performed with ileocecal resection and anisoperistaltic ileocolic anastomosis.
Figure 3 – Intraoperative view showing the ileocecal volvulus with abnormal positioning of the small bowel and colon.
Postoperative recovery was uneventful, and the patient was discharged on postoperative day five. He remained asymptomatic at nine-month follow-up.
DISCUSSION
Intestinal malrotation in adults remains a rare and often under-recognized entity, typically presenting either with vague, intermittent gastrointestinal symptoms or with acute abdominal emergencies such as midgut volvulus (3,6).
In some patients, episodes may be triggered by diet or exertion and are often misattributed to irritable bowel syndrome or functional dyspepsia. The variability in symptoms in this rare condition contributes to diagnostic delays.
Clinical Spectrum and Diagnostic Challenges
Adult presentations of malrotation range from chronic, nonspecific symptoms — such as postprandial discomfort, bloating, and intermittent vomiting — to acute scenarios with bowel obstruction, volvulus, ischemia or perforation. The clinical picture can mimic other disorders, often leading to misdiagnosis or delayed intervention (6,7).
In our case, the patient presented with vomiting, abdominal pain, and obstipation — hallmarks of midgut volvulus.
Role of Imaging
While plain radiography is of limited utility, cross-sectional imaging — particularly contrast-enhanced CT — plays a crucial role in adults. The “whirlpool sign” of twisted mesenteric vessels, malposition of bowel segments, and abnormal location of the duodenojejunal junction are pathognomonic findings (7). In this case, CT imaging was fundamental in achieving a timely diagnosis.
Management Strategies
Surgical correction is the standard of care for symptomatic patients, aiming to relieve obstruction, prevent recurrence, and avoid complications (9). Controversy exists around asymptomatic adults, but most studies advocate surgical correction to prevent catastrophic complications (10).
The classical Ladd procedure remains the cornerstone: it includes counterclockwise detorsion of the bowel, division of peritoneal bands, broadening of the mesenteric root, and appendectomy to avoid future diagnostic confusion (11).
In cases with evidence of ischemia, necrosis, or massive distension, as in our patient, bowel resection may be necessary. While laparoscopic approaches have demonstrated benefits in elective or subacute settings, open surgery continues to be the preferred choice in acute, uncertain, or hemodynamically unstable scenarios (11-13).
Review of Literature and Epidemiological Insights
Intestinal malrotation is primarily recognized as a pediatric condition. The incidence in the general population is estimated at 1 in 500 live births (2), with 85% of symptomatic cases diagnosed within the first year of life, particularly in the neonatal period, where malrotation is a significant surgical emergency (1,4). This early peak reflects the critical consequences of midgut volvulus in infancy, which, if left untreated, can result in extensive bowel necrosis and high mortality and morbidity, including short bowel syndrome and long-term nutritional consequences (14). In neonates, it typically presents with bilious vomiting due to duodenal obstruction, and midgut volvulus is a frequent and feared complication. Most cases are diagnosed early through upper gastrointestinal contrast studies which is considered the gold standard in pediatric populations.
In contrast, adult cases are exceedingly rare, accounting for only 0.2–0.5% of all intestinal obstructions (3). These patients often present with chronic or intermittent symptoms and may go undiagnosed for years. In adults, the absence of specific clinical findings, combined with low suspicion, frequently results in delayed recognition (15).
Published literature reveals a slightly male predominance (M:F – 1.3:1), with most adult patients being diagnosed between the second and fourth decades of life. In a review of 120 adult cases, intermittent abdominal pain was the most common symptom (72%); volvulus occurred in approximately one-third of cases. Diagnostic delays of 6 to 12 months were common from symptom onset. With prompt recognition and surgical management, the prognosis is favorable, with reported mortality below 1% in elective settings, rising to 15–20% when ischemia or perforation are present (7,9,10,12).
Understanding this contrast between pediatric and adult presentations highlights the importance of maintaining a high index of suspicion in adults presenting with unexplained gastrointestinal symptoms, especially when imaging findings raise concern for malrotation (16).
CONCLUSION
Although intestinal malrotation is predominantly a pediatric diagnosis, its occurrence in adults, though rare, should not be overlooked in the differential diagnosis of abdominal symptoms. The condition may remain silent for years or present suddenly with life-threatening complications.
This case reinforces the importance of considering intestinal malrotation in young adults with unexplained gastrointestinal symptoms, especially when imaging reveals atypical bowel positioning or vascular anomalies. Timely diagnosis supported by cross-sectional imaging and definitive surgical management remain vital to avoid adverse outcomes. Raising awareness among clinicians is essential to prevent missed or delayed diagnoses in adult populations.
Conflicts of Interest
No conflicts of interest to declare.
REFERENCES
1. Nehra D, Goldstein AM. Intestinal malrotation: varied clinical presentation from infancy through adulthood. Surgery. 2011;149(3): 386–393.
2. Durkin ET, Lund DP, Shaaban AF, Schurr MJ, Weber SM. Age-related differences in diagnosis and morbidity of intestinal malrotation. J Am Coll Surg. 2008;206(4):658–663.
3. Dietz DW. Intestinal malrotation: a rare but important cause of bowel obstruction in adults. Dis Colon Rectum. 2002;45(10): 1381–1386.
4. Dott NM. Anomalies of intestinal rotation: their embryology and surgical aspects. Br J Surg. 1923;11(43):251–286.
5. Pickhardt PJ, Bhalla S. Intestinal malrotation in adolescents and adults: spectrum of clinical and imaging features. AJR Am J Roentgenol. 2002;179(6):1429–1435.
6. Butterworth WA, Butterworth JW. An adult presentation of midgut volvulus secondary to intestinal malrotation: A case report and literature review. Int J Surg Case Rep. 2018:50:46-49.
7. von Flüe M, Herzog U, Ackermann C, Tondelli P, Harder F. Acute and chronic presentation of intestinal nonrotation in adults. Dis Colon Rectum. 1994;37(2):192–198.
8. Fu T, Tong Y, Wei Y, Li Y. Surgical management of intestinal malrotation in adults. World J Surg. 2007;31(9):1797–1803.
9. Moldrem AW, Papaconstantinou H, Broker H, Megison S, Jeyarajah DR. Late presentation of intestinal malrotation: an argument for elective repair. World J Surg. 2008;32(7):1426–1431.
10. Neville JJ, Gallagher J, Mitra A, Sheth H. Adult Presentations of Congenital Midgut Malrotation: A Systematic Review. World J Surg. 2020;44(6):1771-1778.
11. Zhang X, Xiang L, Qiu T, Zhou J, Che G, Ji Y, et al. Laparoscopic Ladd's procedure for intestinal malrotation in small infants with midterm follow-up. BMC Gastroenterol. 2023;23(1):402.
12. Matzke GM, Moir CR, Dozois EJ. Laparoscopic Ladd procedure for adult malrotation of the midgut with chronic abdominal pain: case report and literature review. J Laparoendosc Adv Surg Tech A. 2003; 13(5):327–329.
13. Johnston WR, Hwang R, Mattei P. Laparoscopic Versus Open Ladd Procedure for Midgut Malrotation. J Pediatr Surg. 2024;59(12): 161673.
14. Torres AM, Ziegler MM. Malrotation of the intestine. World J Surg. 1993;17(3):326–331.
15. Dehaini H, Nasser Eldine R, Doughan S, Khalifeh M, Khasawneh H, Hussain H, et al. Presentation of intestinal malrotation and midgut volvulus in adults: Case report & literature review. Int J Surg Case Rep. 2020:73:27-30.
16. Bostanc? SA, Öztorun C?, Erten EE, Akkaya F, Akbaæ ?, Çayhan VS, et al. Clinical management of intestinal malrotation in different age groups. Pediatr Surg Int. 2024;40(1):204.
Full Text Sources:
Abstract:
Views: 8

For Authors
Journal Subscriptions

Sept 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News