Surgery, Gastroenterology and Oncology

|
|
Introduction: Esophagectomy has a crucial role in the treatment of esophageal cancer. Several different surgical techniques have been performed in order to achieve better post-surgical and oncological outcomes. In this systematic review and meta-analysis, we compare two procedures – Ivor Lewis and McKeown – regarding their impact on morbidity.
Methods: In March 2021, records from Pubmed, Scopus, Web of Science and ClinicalTrials.gov were retrieved. Eligible studies included articles evaluating morbidity outcomes of Ivor Lewis esophagectomy compared to McKeown esophagectomy in patients with resectable esophageal cancer. Main outcomes were postoperative complications, such as anastomotic leak, recurrent laryngeal nerve palsy, chyle leak, respiratory complications; hospital stay length; reoperation and quality of life. A meta-analysis regarding minimally invasive (MI) esophagectomy was performed, using random-effects model.
Results: Sixteen studies with a total of 7339 patients were included in systematic review and eight studies were considered in the meta-analysis, where 3015 patients were enrolled. All the included studies were cohort studies, with a low to moderate risk of bias. The results of the meta-analysis revealed that MIE Ivor-Lewis has a lower incidence of recurrent laryngeal nerve palsy (OR=0.13, 95% CI=0.06-0.31, P= <0.00001), reoperation (OR= 0.60, 95% CI=0.41-0.89, P=0.01), anastomotic leak (OR=0.47, 95% CI=0.28-0.78, P=0.003), and respiratory complications (OR = 0.53, 95% CI = 0.39-0.71, P = <0.0001) when compared to MIE McKeown. There was no statistically significant difference between the two surgical procedures in terms of chyle leak and hospital stay length.
Conclusions: Concerning explored outcomes, MI Ivor Lewis is superior to MI McKeown, except for chyle leak and hospital stay length where no difference was found.
INTRODUCTION
Esophageal cancer (EC) ranks as the eighth most common type of cancer and the sixth most common cause of death worldwide. Its two major forms vary in world distribution – adeno-carcinoma is predominant in western countries while the squamous cell carcinoma is most common in resource-limited countries (1).
In spite of the important role of neoadjuvant therapies, esophagectomy has a major part in the curative treatment of this disease (2). Minimally invasive surgery is progressively increasing in this field, as it is consistently associated with better perioperative outcomes and holds equal survival benefit compared with open esophagectomy. For patients with esophageal tumors above the level of the carina only McKeown is feasible, whereas for patients with lower esophageal or gastroesophageal junction tumors both McKeown and Ivor Lewis procedures are considered to be oncologically effective. However, there is still a lack of data when it comes to what procedure performs superiorly, with more satisfactory outcomes (3-5).
The present article intendes to perform a comprehensive systematic review and meta-analysis of studies comparing Ivor Lewis and McKeown procedures in patients undergoing esophagectomy, in terms of morbidity outcomes.
METHODS
Literature search strategy
This systematic review and meta-analysis follow the principles set in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement (6).
Pubmed, Scopus, ClinicalTrials.gov and Web of Science were searched in March 2021 using the following query: (“oesophagus” OR “esophagus” OR “esophageal”) AND (“cancer” OR “carcinoma”) AND (“Ivor Lewis” OR “Ivor-Lewis”) AND “McKeown”.
Eligibility criteria and study selection
Inclusion criteria were as follows: (I) studies published between 2015 and 2021; (II) randomized clinical trials, either prospective or retrospective cohort studies and case-control studies; (III) studies comparing patients with esophageal cancer (any esophageal location or Siewert types I or II gastroesophageal junction cancers) submitted to Ivor Lewis and McKeown esophagectomy; (IV) morbidity outcomes, defined as hospital stay length, short and long-term surgical complications, reoperation, and quality of life. Exclusion criteria were as follows: (I) reviews, case-reports, letters to editor, surveys and animal studies; (II) language other than English / Portuguese / Spanish; (III) Studies without full-text available; (IV) studies with less than 10 patients.
All searching records were divided between two groups of two reviewers – group one (FS and IC), and group two (NP and SS) – who first independently screened titles and abstracts for inclusion. Subsequently, the considered studies were downloaded in full-text format and were assessed by the same group of reviewers. Disagreements were resolved either by consensus or consultation with a third reviewer from the other group. This process is described in a flowchart according to the PRISMA statement (6).
Data extraction process
Using a data extraction table, the required information was looked up in the text, tables, and figures by the two groups of reviewers (FS and IC; NP and SS) independently. The data included: (I) paper information: first author’s name, year of publication, country, study’s duration and study design; (II) characteristics of the samples: numbers of included patients, carcinoma location and histology; (III) type of surgical technique compared (open, hybrid or minimally invasive surgery); (IV) morbidity outcome parameters.
Quality assessment
Newcastle-Ottawa quality assessment scale (NOS) (7) was used to assess the quality of all included cohort studies. The same two groups of reviewers scored independently each of the studies. The scale comprises 8 items divided into three parts: selection (representative, selection, ascertainment of exposure and demonstration, with maximum score of 4 points), comparability (maximum score of 2 points), and outcome (outcome, follow-up and adequacy of follow-up, with a maximum score of 3 points). The adequacy of follow-up was considered when >80% of follow-up was achieved.(8) Therefore, a maximum score of 9 points, reflects the highest quality.
Statistical analysis
Meta-analysis was performed using Review Manager 5.4 software. Six outcomes were pooled for meta-analysis and represented in forest plots, including: hospital length stay, anastomotic leak, recurrent laryngeal nerve palsy, respiratory complications, chyle leak and reoperation. Heterogeneity was assessed using the Cochran Q and the I2 statistic. A p < 0.05 or an I2 value >50% were considered substantial heterogeneity; therefore, subgroup analysis and sensitivity analysis (leave-one-out approach) would be performed, if necessary. Regardless of the heterogeneity, random-effects model was always employed, thereby obtaining more conservative results. Regarding effect measures, for dichotomic parameters, odds ratios (OR) with 95% confidence intervals (CI) were calculated and for continuous parameters, mean difference with 95% CI were used. p < 0.05 was considered statistically significant. Publication bias was evaluated visually through funnel plots.
RESULTS
Study selection
The systematic literature screening and selection process is demonstrated in detail in fig. 1.
Figure 1 – PRISMA based flowchart

We retrieved 391 publications from the databases after duplicates removal, which were then screened regarding title and abstract. 351 were excluded because of inadequacy to our searching goal, and 40 were full text assessed for eligibility. 16 of these matched the inclusion criteria. For the meta-analysis, 7 studies and 1 study’s sub-analysis were included, as only these conveyed concrete data for Minimally Invasive (MI) esophagectomy. This sub-analysis is part of an article by Sabra(9) who found no differences between open and minimally invasive surgery. Nevertheless, this same author managed to perform a sub-analysis of the initial population regarding only patients submitted to MIE, with this data being included in this meta-analysis.
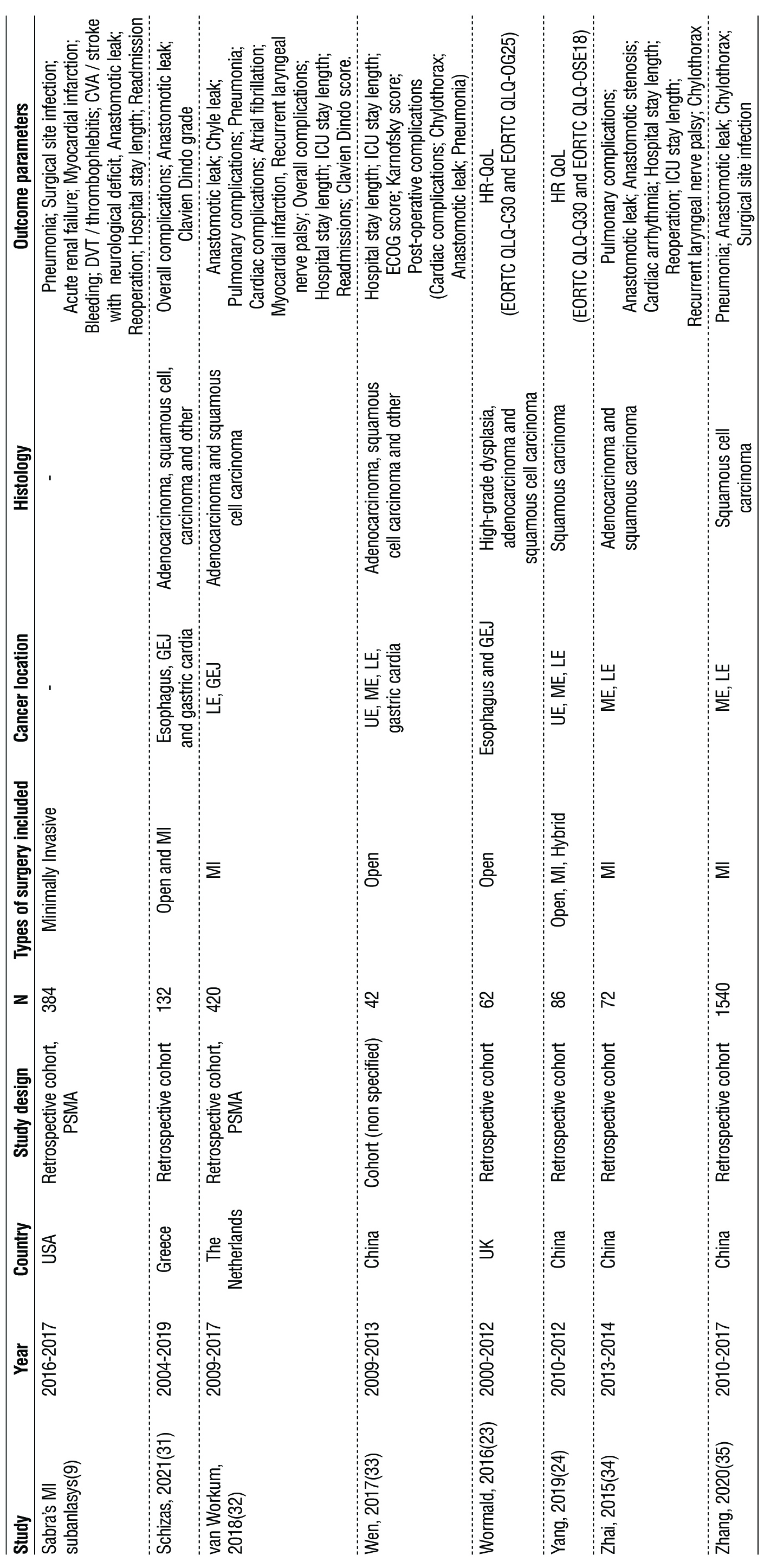
Study characteristics
All studies’ extracted data and further related information can be found in table 1. The studies had a number of patients varying from 42 to 3268. In 8 studies (n = 3015), MI Ivor Lewis was compared to MI McKeown, thus having been included in the meta-analysis. In the 9 remaining studies, different techniques were explored: in 3 studies (n = 306) the these techniques were analyzed as open surgery procedures; 4 studies (n = 3829) included the comparison of open surgery with minimal invasive techniques regarding both Ivor Lewis and McKeown procedures; 2 studies (n = 573) provided results of hybrid McKeown opposed to open Ivor Lewis (n = 487) and, in a more broaden spectrum, of the three techniques – open, minimally invasive and hybrid – concerning Ivor Lewis and McKeown (n = 86).
Table 1 – Characteristics of the included studies. CVA – cerebral vascular accident; DVT – deep venous thrombosis; ECOG - Eastern Cooperative Oncology Group; EORTC QLQ - European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire; GEJ – gastro oesophageal junction; HR-QoL - Health-related quality of life; ICU – intensive care unit; IL – Ivor Lewis; LE – lower esophagus; LOS – Length of stay; McK – McKeown; ME – middle esophagus; MI – minimally invasive; PSMA – prospective score matched analysis; RLN – recurrent laryngeal nerve; UE – upper esophagus.

Relevant outcomes not suitable for meta-analysis
A detailed description of the more important sought outcomes is showed in table 2 and all the others are in Supplementary table 1. Owing to the fact that several studies reported a vast range of cardiac complications, we considered utterly pertinent to describe them - even though they were not appropriate for meta-analysis due to the rather heterogenous measured parameters, its clinical relevance should not be ignored. Regarding nonspecific cardiovascular complications (acute kidney injury and conduit necrosis/ leak) no differences between Ivor Lewis and McKeown were found in any of the included studies.
Table 2 – Parameters evaluated in included studies. Data is listed as follows:
Ivor Lewis / McKeown. ECOG - Eastern Cooperative Oncology Group; EORTC QLQ - European Organization for the Research and Treatment of Cancer Quality of Life Questionnaire; IL – Ivor Lewis; LOS – length of stay; McK – McKeown; QoL – Quality of Life; RLN – recurrent laryngeal nerve.

Supplementary table 1 – Outcomes of the included studies. MI – Minimally invasive;

IL – Ivor-Lewis; McK - McKeown
Concerning global quality of life, no differences between Ivor-Lewis and McKeown were found in any individual study. Only Barbour et al (10) found that the mean symptoms score for pain is higher in patients who underwent open transthoracic Ivor Lewis esophagectomy after 2 years follow-up. Finally, no differences between Ivor-Lewis and McKeown were found in any individual study for anorexia.
Quality and risk of bias assessment
Taking into consideration that no randomized trials were found, the Newcastle-Ottawa rating scale was applied to each study individually for risk of bias assessment (Supplementary table 2). 15 in 16 studies scored 7 or more points, corresponding to a low risk of bias. One scored 6 points, corresponding to a moderate risk of bias. This was a retrospective cohort study, with 86 patients. Comparability was the parameter less scored, found within 7 studies.
Supplementary table 2 – Newcastle-Ottawa rating scale for quality and risk of bias assessment

In the article by Ericson et al (11), one of the parameters - follow-up - could not be evaluated, due to lack of information attributable to the loss of participants during the follow-up period of the study. Since this study had a retrospective cohort, there could have been some selection bias, with only the patients whose follow-up was complete being included.
Meta-analysis
The results of meta-analysis are displayed in fig. 2. Anastomotic leak was reported in eight studies including 3015 patients, recurrent laryngeal nerve palsy in six studies including 1091 patients, chyle leak in six studies including 2446 subjects, respiratory complications in six studies including 1091 patients, hospital stay length in studies including 760 patients and reoperation in 5 studies including 1180 subjects. respiratory complications in six studies including 1091 patients, hospital stay length in studies including 760 patients and, finally, reoperation in 5 studies including 1180 subjects. Comparing to MI McKeown, MI Ivor-Lewis has a statistically significant lower incidence of recurrent laryngeal nerve palsy (OR = 0.13, 95% CI = 0.06-0.31, P = <0.00001), reoperation (OR = 0.60, 95% CI = 0.41-0.89, P = 0.01), anastomotic leak (OR = 0.47, 95% CI = 0.28-0.78, P = 0.003), and respiratory complications (OR = 0.53, 95% CI = 0.39-0.71, P = <0.0001). There was no statistically significant difference between the two surgical procedures in terms of chyle leak (OR = 0.74, 95% CI = 0.43-1.29, P = 0.29) and hospital stay length (mean difference = -1.23; 95% CI = -2.55-0.10, P = 0.07). No substantial heterogeneity was detected.
Figure 2 – Meta-analysis forest plots. (a) – Hospital Stay Length; (b) - Recurrent laryngeal nerve palsy; (c) – Chyle Leak; (d) – Reoperation; (e) – Anastomotic Leak; (f) – Respiratory complications.

In order to assess publication bias, funnel plots were constructed and are presented in fig. 3. The studies’ distribution was fairly symmetrical for anastomotic leak, chyle leak and respiratory complications.
Figure 3 – Meta-analysis funnel plots. (a) – Hospital Stay Length; (b) RLN palsy (c) - Chyle Leak;
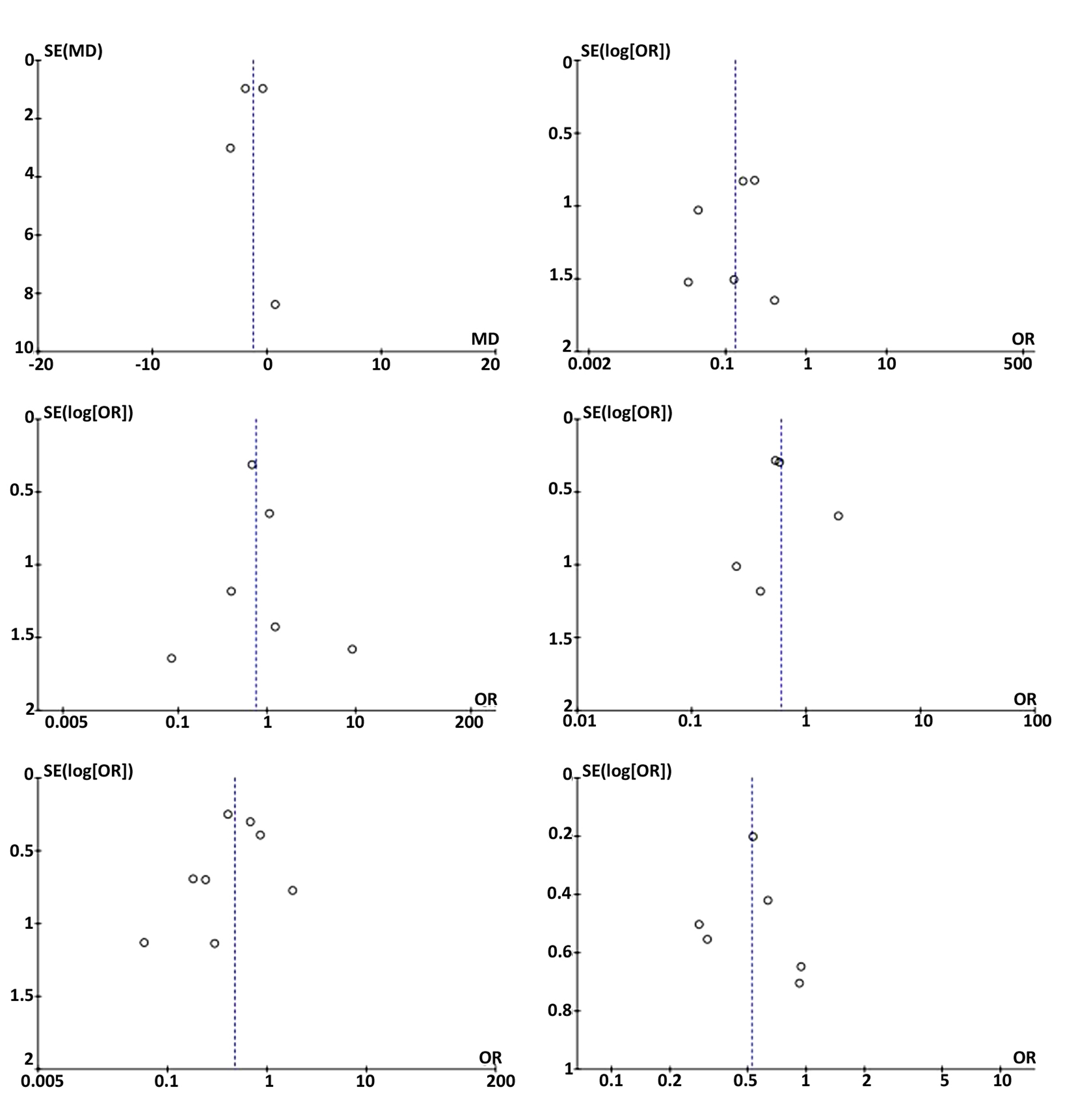
(d) – Reoperation; (e) – Anastomotic Leak; (f) – Respiratory complications.
DISCUSSION
It has already been established that a minimally invasive approach can result in better postoperative outcomes (12) when compared to open procedures with similar oncological results (13). Hence our option to only consider patients in whom minimally invasive esophagectomy was performed.
When analyzing hospital stay length, the mean difference was not statistically significant. While this is a commonly considered aspect when exploring the results of a surgical technique, one must consider that it can also result from established protocols instead of it meaning morbidity. These results are different from those presented by other authors (14), who favor the Ivor-Lewis technique, as it may result in less recurrent laryngeal nerve injury and less blood loss.
Similarly to other meta-analysis (3,14), our data shows a lower incidence of recurrent laryngeal nerve injury in the Ivor-Lewis procedure. This is mainly related to the fact that the McKeown technique implies a cervical dissection and anastomosis, which can result in an iatrogenic injury.
Regarding chyle leak, no statistically significant differences were found. The fact that the thoracic duct is close to the esophagus makes this event possible. Possible risk factors for chyle leak have been reported by other authors, including preoperative chemoradiotherapy and high intraoperative fluid balance (15,16).
The need for reoperation was reported in five of the studies. Our findings favor, with a statistically significant result, the Ivor Lewis intervention. The higher reoperation rate in the McKeown procedure may be a result of the sum of all the post-operative complications. While it is true that thoracic anastomotic leaks are more prone to surgical re-exploration (17) while a leak on a cervical anastomosis can be treated by using wet-to-dry dressing changes, (18) the lower percentage of leaks found in the Ivor Lewis procedure may justify these numbers.
We found that there was a lower incidence of anastomotic leak with Ivor Lewis MIE. Similar results have been suggested, (5) albeit with no statistically significant differences were found, possibly related a smaller number of participants included (1681 vs 3015). Possible explanations for this are a better healing of intrathoracic anastomosis due to better vascularization and the lower level of the gastric tube with consequential reduce tension at the anastomosis (3). As much as the anastomotic technique (handsewn or stappled) may also influence the data, (19) not every report described the surgical procedures and such was not considered. This fact may also be responsible for the high percentage of heterogeneity observed.
Lastly, our meta-analysis contemplated respiratory complications among patients submitted to esophagectomy. Some authors (20) observed a lower incidence of negative respiratory outcomes in minimaly invasive techniques, but studies lack comparing both Ivor Lewis and McKeown surgeries. Our data states Ivor Lewis surgery is associated with a lower rate of respiratory complications, which might be explained by the higher risk of RLN lesion in McKeown’s surgery (21), increasing the risk of aspiration.
Not only efficacy and safety are crucial in surgical oncology, but also quality of life. Even more since, esophagectomy is an aggressive surgery and patients with esophageal cancer are diagnosed in advanced stages, having thereby an unfavorable prognosis. Our findings suggested that global quality of life is similar between the two procedures. No meta-analysis was conducted, since the four included studies had different surgical approaches (10,22-24) Therefore, any results favoring either Ivor-Lewis or McKeown could be biased and be explained by the aggressiveness of open surgery and not the type of the esophagectomy made.
Publication bias assessment was not possible for all outcomes, since the number of studies included was not sufficient to build a funnel plot from which conclusions could be taken. Nevertheless, we can assume that for anastomotic leak, chyle leak and respiratory complications there was not any publication bias.
It is relevant to remark that most studies included in this systematic review were retrospective studies, which may induce some selection bias.
Additionally, there was a general lack of concept’s definitions, namely (a) the esophagus anatomic zones’ division (not uniform between studies), (b) the evaluated parameters (for instance, the concept of ‘Respiratory Complications’ or ‘Cardiovascular Complications’ might not be as homogeneous as desirable), and (c) the description of the surgical procedures themselves. In some articles, the authors mention both McKeown and Ivor Lewis techniques, without proper detail (21,25).
Of the 16 included reports, only about four used a score allowing severity complications comprehension (26). With its use being evermore frequent, more precise results may be determined in the future when comparing Ivor-Lewis and McKeown procedures.
CONCLUSION
Concerning explored outcomes, MI Ivor Lewis is superior to MI McKeown, except for chyle leak and hospital stay length where no difference was found. This should be interpreted with caution since only cohort studies could be included. Nevertheless, when considering partial esophagectomy in patients were both techniques are feasible, Ivor-Lewis appears to present better results in terms of less recurrent laryngeal nerve injury, need for reoperation, anastomotic leaks and respiratory complications.
Conflict of interest
All author declare that they have no conflict of interest.
Funding
No funding sources.
REFERENCES
1. Napier KJ, Scheerer M, Misra S. Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol. 2014;6(5):112-20.
2. Shah MA, Kennedy EB, Catenacci DV, Deighton DC, Goodman KA, Malhotra NK, et al. Treatment of Locally Advanced Esophageal Carcinoma: ASCO Guideline. J Clin Oncol. 2020;38(23):2677-94.
3. Deng J, Su Q, Ren Z, Wen J, Xue Z, Zhang L, et al. Comparison of short-term outcomes between minimally invasive McKeown and Ivor Lewis esophagectomy for esophageal or junctional cancer: a systematic review and meta-analysis. Onco Targets Ther. 2018; 11:6057-69. eCollection 2018.
4. Wang J, Hu J, Zhu D, Wang K, Gao C, Shan T, et al. McKeown or Ivor Lewis minimally invasive esophagectomy: a systematic review and meta-analysis. Transl Cancer Res. 2020;9(3):1518-27.
5. van Workum F, Berkelmans GH, Klarenbeek BR, Nieuwenhuijzen GAP, Luyer MDP, Rosman C. McKeown or Ivor Lewis totally minimally invasive esophagectomy for cancer of the esophagus and gastroesophageal junction: systematic review and meta-analysis. J Thorac Dis. 2017;9(Suppl 8):S826-s33.
6. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Bmj. 2009;339:b2700.
7. Wells GA, Wells G, Shea B, Shea B, O'Connell D, Peterson J, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2014.
8. National Heart LaBI. Study Quality Assessment Tools 2021 [updated July, 2021. Available from: https://www.nhlbi.nih.gov/health-topics /study-quality-assessment-tools.
9. Sabra MJ, Alwatari YA, Wolfe LG, Xu A, Kaplan BJ, Cassano AD, et al. Ivor Lewis vs Mckeown esophagectomy: analysis of operative outcomes from the ACS NSQIP database. Gen Thorac Cardiovasc Surg. 2020;68(4):370-9.
10. Barbour AP, Cormack OMM, Baker PJ, Hirst J, Krause L, Brosda S, et al. Long-term Health-related Quality of Life Following Esophagectomy: A Nonrandomized Comparison of Thoracoscopically Assisted and Open Surgery. Ann Surg. 2017;265(6):1158-65.
11. Ericson J, Lundell L, Klevebro F, Kamiya S, Nilsson M, Rouvelas I. Long-term weight development after esophagectomy for cancer-comparison between open Ivor-Lewis and minimally invasive surgical approaches. Dis Esophagus. 2019;32(4):doy075.
12. Mariette C, Markar SR, Dabakuyo-Yonli TS, Meunier B, Pezet D, Collet D, et al. Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer. N Engl J Med. 2019;380(2):152-62.
13. Sihag S, Wright CD, Wain JC, Gaissert HA, Lanuti M, Allan JS, et al. Comparison of perioperative outcomes following open versus minimally invasive Ivor Lewis oesophagectomy at a single, high-volume centre†. Eur J Cardiothorac Surg. 2012;42(3):430-7.
14. van Workum F, Klarenbeek BR, Baranov N, Rovers MM, Rosman C. Totally minimally invasive esophagectomy versus hybrid minimally invasive esophagectomy: systematic review and meta-analysis. Dis Esophagus. 2020;33(8):doaa021.
15. Yoshida N, Baba H. Risk factors for chylothorax after esophagectomy. J Thorac Dis. 2019;11(Suppl 3):S196-s7.
16. Chen S, Zhao Y, Chen H. Risk factors of chylothorax after esophagectomy. J Thorac Dis. 2019;11(5):1749-52.
17. Baba M, Aikou T, Natsugoe S, Kusano C, Shimada M, Kimura S, et al. Appraisal of ten-year survival following esophagectomy for carcinoma of the esophagus with emphasis on quality of life. World J Surg. 1997;21(3):282-5; discussion 6.
18. Swanson SJ, Batirel HF, Bueno R, Jaklitsch MT, Lukanich JM, Allred E, et al. Transthoracic esophagectomy with radical mediastinal and abdominal lymph node dissection and cervical esophago-gastrostomy for esophageal carcinoma. Ann Thorac Surg. 2001; 72(6):1918-24; discussion 24-5.
19. Ozawa S, Koyanagi K, Ninomiya Y, Yatabe K, Higuchi T. Postoperative complications of minimally invasive esophagectomy for esophageal cancer. Ann Gastroenterol Surg. 2020;4(2):126-34.
20. Findlay L, Yao C, Bennett DH, Byrom R, Davies N. Non-inferiority of minimally invasive oesophagectomy: an 8-year retrospective case series. Surg Endosc. 2017;31(9):3681-9.
21. Luketich JD, Pennathur A, Awais O, Levy RM, Keeley S, Shende M, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg. 2012;256(1):95-103.
22. Jezerskyte E, Saadeh LM, Hagens ERC, Sprangers MAG, Noteboom L, van Laarhoven HWM, et al. Long-term health-related quality of life after McKeown and Ivor Lewis esophagectomy for esophageal carcinoma. Dis Esophagus. 2020;33(11):doaa022.
23. Wormald JC, Bennett J, van Leuven M, Lewis MP. Does the site of anastomosis for esophagectomy affect long-term quality of life? Dis Esophagus. 2016;29(1):93-8.
24. Yang YS, Shang QX, Yuan Y, Wu XY, Hu WP, Chen LQ. Comparison of Long-term Quality of Life in Patients with Esophageal Cancer after Ivor-Lewis, Mckeown, or Sweet Esophagectomy. J Gastrointest Surg. 2019;23(2):225-31.
25. Kohli AA, Noor; Mir, Ishtayak A. Esophagectomy for Cancer of the Esophagus-GMC Jammu Experience. JK Science. 2020;22(1):3-6.
26. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187-96.
27. Brown AM, Pucci MJ, Berger AC, Tatarian T, Evans NR, 3rd, Rosato EL, et al. A standardized comparison of peri-operative complications after minimally invasive esophagectomy: Ivor Lewis versus McKeown. Surg Endosc. 2018;32(1):204-11.
28. Chang T, Hsiao PN, Tsai MY, Huang PM, Cheng YJ. Perioperative management and outcomes of minimally invasive esophagectomy: case study of a high-volume tertiary center in Taiwan. J Thorac Dis. 2018;10(3):1670-6.
29. Chen L, Liu X, Wang R, Wang Y, Zhang T, Gao D, et al. Minimally invasive esophagectomy for esophageal cancer according to the location of the tumor: Experience of 251 patients. Ann Med Surg (Lond). 2017;17:54-60.
30. Hou XB, Ren ZP, Yang B, Liu Y. Comparison of short- term therapeutic efficacy between minimally invasive Ivor- Lewis esophagectomy and Mckeown esophagectomy for esophageal cancer. Biomedical Research-India. 2017;28(12):5321-6.
31. Schizas D, Mylonas KS, Hasemaki N, Mpaili E, Ntomi V, Michalinos A, et al. Esophageal cancer surgery in Greece during the era of the financial crisis. Dis Esophagus. 2021;34(2):doaa067.
32. van Workum F, Slaman AE, van Berge Henegouwen MI, Gisbertz SS, Kouwenhoven EA, van Det MJ, et al. Propensity Score-Matched Analysis Comparing Minimally Invasive Ivor Lewis Versus Minimally Invasive Mckeown Esophagectomy. Ann Surg. 2020;271(1):128-33.
33. Wen SW, Han L, Zhang YF, Tian ZQ, Li Y, Lv HL, et al. Comparison of survival rate, complications and life quality after different surgical procedures in esophageal cancer. International Journal of Clinical and Experimental Pathology. 2017;10(2):1886-97.
34. Zhai C, Liu Y, Li W, Xu T, Yang G, Lu H, et al. A comparison of short-term outcomes between Ivor-Lewis and McKeown minimally invasive esophagectomy. J Thorac Dis. 2015;7(12):2352-8.
35. Zhang T, Hou X, Li Y, Fu X, Liu L, Xu L, et al. Effectiveness and safety of minimally invasive Ivor Lewis and McKeown oesophagectomy in Chinese patients with stage IA-IIIB oesophageal squamous cell cancer: a multicentre, non-interventional and observational study. Interact Cardiovasc Thorac Surg. 2020;30(6):812-9.
Full Text Sources:
Abstract:
Views: 3337

For Authors
Journal Subscriptions

Jun 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News