Surgery, Gastroenterology and Oncology
|
|
ABSTRACT
Background: This retrospective comparative study evaluated the impact of wound edge protector use on surgical site infection (SSI) rates in patients undergoing open appendectomy for acute appendicitis.
Methods: Medical records from Vajira Hospital (2020–2023) were reviewed. Propensity score matching was used to adjust for baseline characteristics. All patients received peri-operative intravenous antibiotics and 4% chlorhexidine antiseptic skin preparation. Outcomes including SSI, blood loss, pain scores, and hospital stay were analysed using chi-square test and logistic regression.
Results: Among the 125 patients, 58 underwent surgery with a wound edge protector, and 67 without. Following matching, the SSI rate was significantly lower in the wound edge protector group (9.43%) compared to the non-protector group (28.85%) (p < 0.05). The protector group also experienced reduced blood loss, lower postoperative pain scores, and shorter hospital stays.
Conclusion: Use of a wound edge protector in open appendectomy was associated with lower SSI risk and improved perioperative outcomes. While the findings are promising, the retrospective design and potential residual confounders warrant validation through prospective randomised studies.
INTRODUCTION
Acute appendicitis is among the most common abdominal emergencies, with appendectomy as the standard treatment. Although appendectomy is a relatively safe procedure, surgical site infection (SSI) remains a frequent post-operative complication, contributing to extended hospital stays, higher healthcare costs, and decreased quality of life for patients (1-3). The pathophysiology of SSI is complex and multifactorial, primarily involving endogenous pathogens from the skin or gastrointestinal tract, making intraoperative contamination a major determinant of SSI rates (4-6). SSI rates vary depending on the complexity of appendicitis, ranging from less than 5% in uncomplicated cases to as high as 20% in cases with perforated or gangrenous appendicitis (7).
Efforts to prevent SSI include a range of strategies, such as preoperative antibiotics, antiseptic skin pre-paration, and maintaining a sterile environment at the wound edges during surgery (8-10). One device that has gained attention in this context is the wound edge protector, a simple and easy-to-use tool designed to reduce contamination at the incisional wound edges (11-13).
The effectiveness of wound edge protectors in reducing SSI has been explored in several studies with mixed results. Some research has demonstrated a significant reduction in SSIs with the use of wound edge protectors (14,15) while other studies found that protectors reduce superficial but not deep infections (16). The variation in findings suggests that further investigation is warranted to clarify the protector's role in minimizing SSI risks in open appendectomy.
This study aims to evaluate the efficacy of wound edge protectors in reducing SSIs among patients undergoing open appendectomy for acute appendicitis.
By comparing outcomes between groups with and without the device, this study seeks to contribute valuable insights into SSI prevention strategies for appendectomy.
Materials and Methods
Study Design and Ethics
This was a retrospective comparative study conducted at the Department of Surgery, Faculty of Medicine Vajira Hospital, Navamindradhiraj University. Ethical approval was obtained from the Vajira Institutional Review Board (IRB No. COA 31/2558). The requirement for informed consent was waived due to the retrospective nature of the study.
Study Population
The study included patients who underwent open appendectomy for acute appendicitis between January 2020 and December 2023. Inclusion criteria were patients aged 18 to 60 years with a confirmed diagnosis of acute appendicitis. Exclusion criteria included immuno-compromised status (e.g., receiving chemo-therapy, long-term steroids), pre-existing wound infections, pregnancy, or conversion to laparoscopic appendectomy.
Group Allocation
Patients were categorised into two groups based on the surgical technique documented in the operative notes. The wound edge protector group consisted of patients in whom the device was applied after peritoneal entry. The non-protector group underwent appendectomy without the use of a wound edge protector. Group allocation was determined by surgeon preference and standard operating practice during the study period.
Data Collection and Baseline Characteristics
Clinical data were retrieved from inpatient, out-patient, and operative records. Baseline characteristics included age, sex, body mass index (BMI), comorbidities (e.g., diabetes mellitus, hypertension), and appendicitis severity. Intraoperative details such as operative time and estimated blood loss were also recorded.
Propensity Score Matching
To reduce selection bias, propensity score matching (PSM) was performed using logistic regression based on key baseline covariates, including age, sex, BMI, comorbidities, and severity of appendicitis. A 1:1 nearest-neighbour matching without replacement was conducted using a caliper width of 0.2. The resulting matched groups were used for subsequent statistical comparison.
Surgical Procedure and Infection Control Protocols
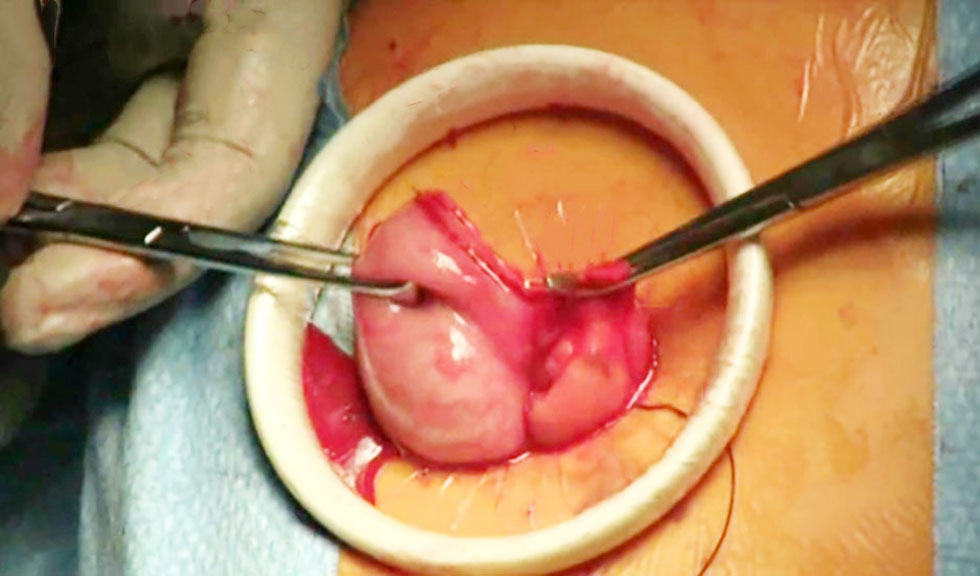
All patients received preoperative intravenous antibiotics (cefoxitin 2 g) and underwent antiseptic skin preparation with 4% chlorhexidine gluconate. The surgical approach involved a standard right lower quadrant muscle-splitting incision (Lanz incision). In the wound edge protector group, a flexible double-ring protector was placed following peritoneal entry and removed prior to closure. Saline irrigation and primary layered closure were performed in both groups.
Outcome Measures
The primary outcome was the incidence of surgical site infection (SSI) within 30 days postoperatively, defined according to the US Centers for Disease Control and Prevention (CDC) criteria. SSI was diagnosed based on erythema, swelling, tenderness, purulent discharge, or positive wound culture. Secondary outcomes included estimated blood loss (ml), postoperative pain (measured via Visual Analog Scale, VAS), time to ambulation, time to first oral intake, and length of hospital stay (days).
Statistical Analysis
Descriptive statistics were summarised as mean ± standard deviation or median (interquartile range), as appropriate. Categorical variables were compared using chi-square or Fisher’s exact test, and continuous variables were analysed with the Student’s t-test or Mann-Whitney U test. A p-value < 0.05 was considered statistically significant. All analyses were performed using STATA version 16.0 (StataCorp LLC, College Station, TX, USA).
Figure 1 - Use of wound edge protector during open appendectomy showing ring placement at incision edge
Results
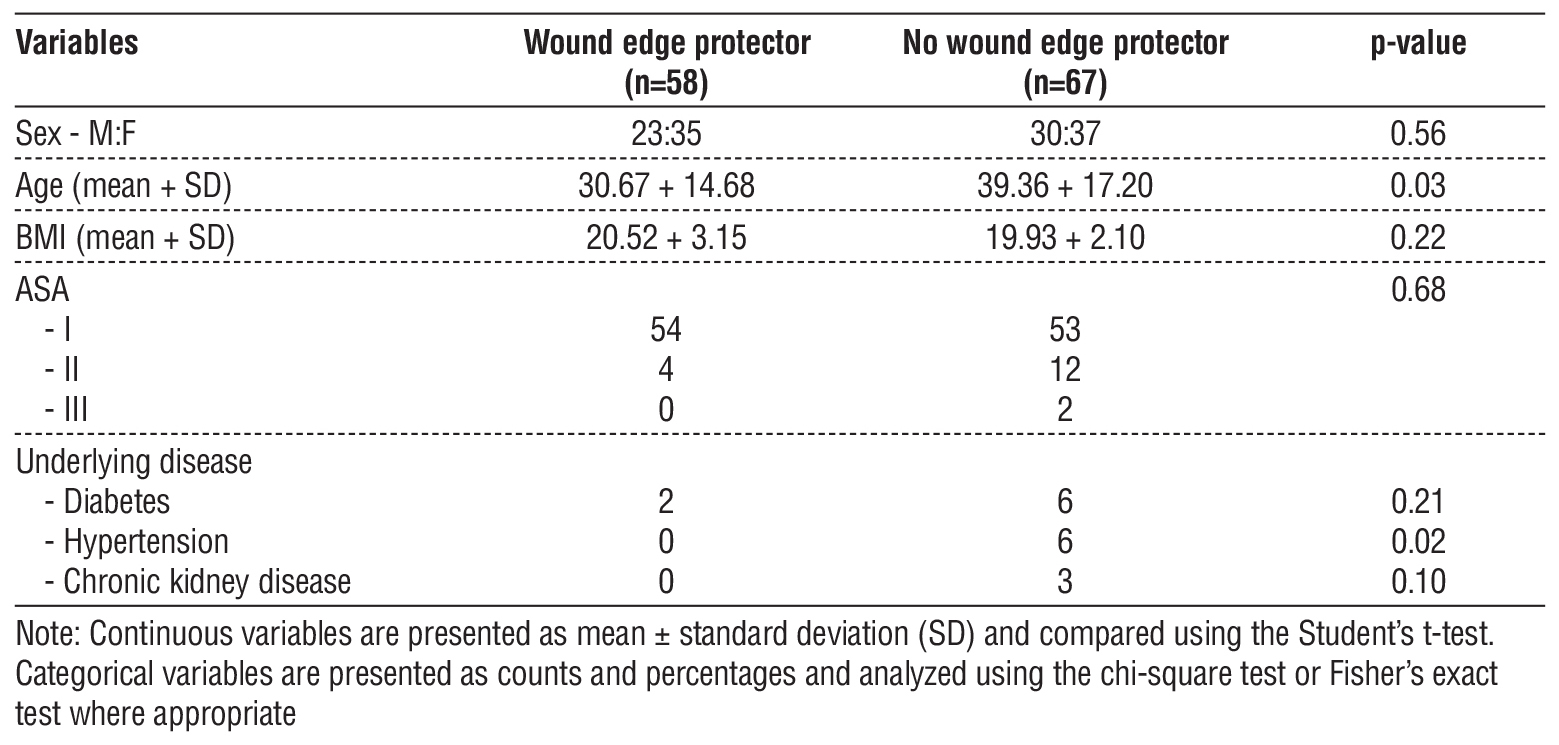
A total of 125 patients were included in the analysis, with 58 patients in the wound edge protector group and 67 patients in the non-wound edge protector group. Propensity score matching was performed using key baseline characteristics including age, sex, body mass index (BMI), and comorbidities such as diabetes and hypertension, resulting in two balanced groups. This matching process helped to balance potential confounding factors and minimize bias in comparing outcomes between the two groups.
Following matching, no statistically significant differences were observed in baseline characteristics between the two groups (table 1). This confirmed adequate matching and allowed for valid outcome comparisons.
Table 1 - Baseline characteristics of the study population
Primary Outcome
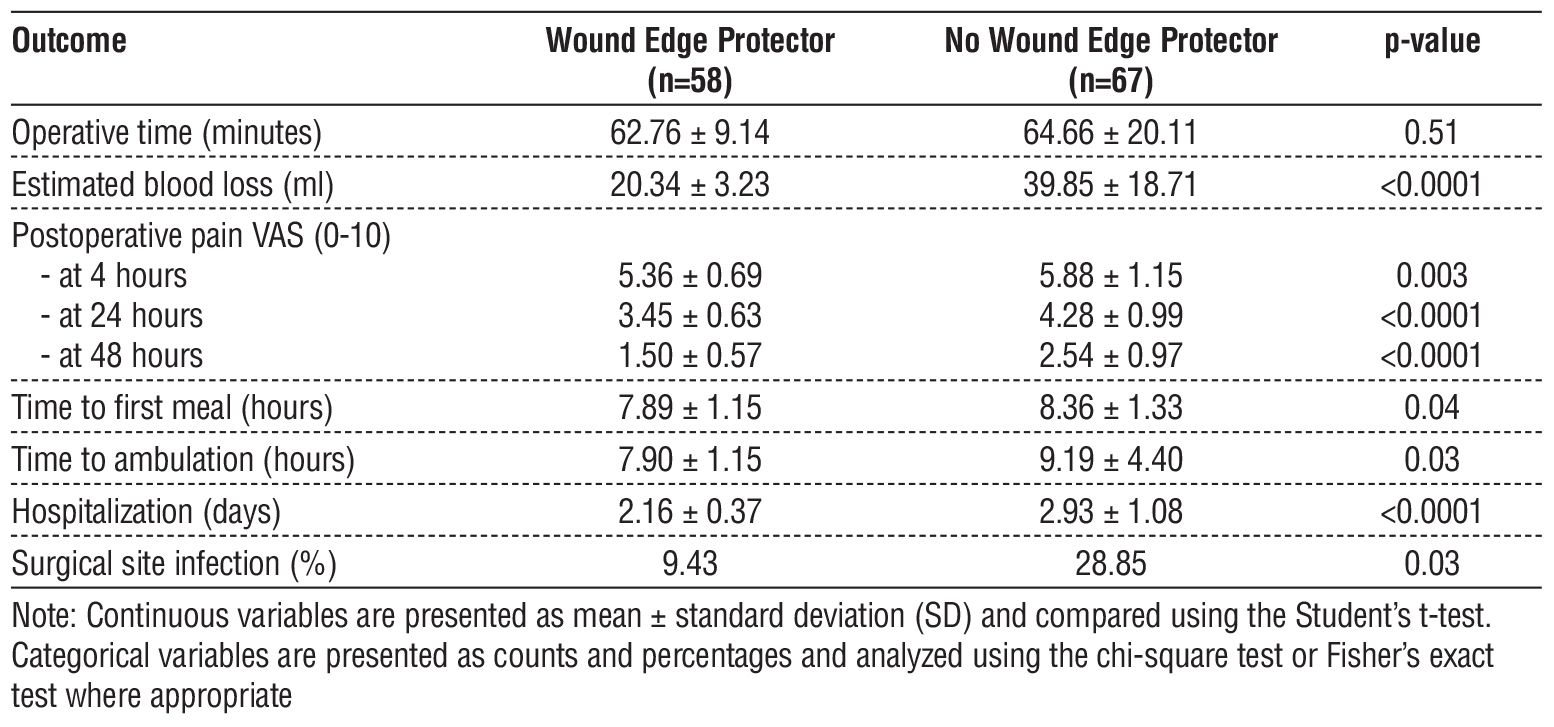
The incidence of surgical site infection (SSI) was significantly lower in the wound edge protector group (9.43%) compared to the non-wound edge protector group (28.85%) (p = 0.03).
Secondary Outcomes
In addition to the reduction in surgical site infections, the wound edge protector group demonstrated favourable perioperative outcomes across multiple parameters. The estimated intraoperative blood loss was significantly lower in patients who received a wound edge protector, with a mean volume of 20.34 ± 3.23 millilitres, compared to 39.85 ± 18.71 millilitres in the non-protector group (p < 0.0001).
Postoperative pain scores, assessed using the Visual Analog Scale, were consistently lower in the wound edge protector group at all measured time points. At 4 hours postoperatively, the pain score was significantly reduced (p = 0.003), with further reductions observed at 24 hours (p < 0.0001) and 48 hours (p < 0.0001) compared to the control group.
Recovery parameters also favoured the wound edge protector group. The time to first oral intake was shorter, averaging 7.89 ± 1.15 hours, compared to 8.36 ± 1.33 hours in the non–protector group (p = 0.04). Similarly, the time to ambulation was reduced (7.90 ± 1.15 hours vs. 9.19 ± 4.40 hours, p = 0.03).
Furthermore, the length of hospital stay was significantly shorter among patients in the wound edge protector group, with an average duration of 2.16 ± 0.37 days, compared to 2.93 ± 1.08 days in those who did not receive the device (p < 0.0001). These perioperative benefits are detailed in table 2.
Table 2 - Operative Outcomes after Propensity Score Matching
DISCUSSION
This study demonstrates that the use of a wound edge protector during open appendectomy was associated with a significantly lower rate of surgical site infection (SSI) compared to procedures performed without the device. The application of propensity score matching to adjust for baseline differences strengthened the internal validity of the analysis by reducing selection bias. The primary outcome, SSI rate, was notably lower in the wound edge protector group (9.43%) than in the non-protector group (28.85%), which is in agreement with multiple prior studies supporting the benefit of wound edge protectors in reducing intraoperative contamination (14,15).
The observed reduction in SSIs is likely attributable to the protector’s role in shielding the incision from exposure to contaminated tissues. SSIs frequently arise from endogenous skin or gastrointestinal flora introduced during intra-abdominal procedures (17). By serving as a mechanical barrier, the wound edge protector helps prevent direct contact between contaminated viscera and the wound edges, thereby lowering the risk of bacterial infiltration and sub-sequent infection.
Our results are in line with those reported by Mihaljevic et al. (18) and Horiuchi et al. (19), who reported lower SSI rates in surgeries utilizing wound edge protectors. While some studies indicate that wound edge protectors may primarily reduce superficial SSIs, this study’s findings suggest a broader benefit, including deeper infection prevention. The lower rates of postoperative pain, shorter recovery times, and reduced hospital stay further underscore the advantages of wound edge protectors in open appendectomy. The consistent reduction in pain scores at different postoperative intervals may suggest that minimized wound contamination correlates with reduced inflammatory response and associated discomfort.
In addition to a lower incidence of SSIs, the wound edge protector group demonstrated improved peri-operative recovery. These patients experienced less intraoperative blood loss, earlier ambulation, a shorter time to first oral intake, and reduced length of hospital stay. Together, these outcomes may translate into lower rates of postoperative complications, faster return to baseline function, and reduced healthcare resource utilisation. This observation aligns with the findings of De Pastena et al. (10), who also reported lower hospitalisation costs associated with reduced infection rates when wound edge protectors were employed.
This study has limitations inherent to its retrospective, quasi-experimental design. While propensity score matching was used to reduce selection bias, a randomized controlled trial (RCT) would provide a higher level of evidence to confirm the observed benefits of wound edge protectors in SSI prevention. Additionally, our study was limited to a single center, which may limit the generalizability of the findings to other patient populations and surgical settings. Future RCTs with larger sample sizes across multiple centers could validate these results and explore specific types of SSIs (e.g., superficial vs. deep) that wound edge protectors may affect differentially.
Nevertheless, certain limitations must be acknowledged. First, this was a retrospective, single-centre study, which inherently limits generalisability. Second, despite the use of propensity score matching, residual confounding cannot be excluded. Third, we did not stratify SSI outcomes by type (e.g. superficial vs. deep), which may be relevant in clarifying the mechanism of protection. A multicentre randomised controlled trial with stratified SSI analysis would provide more definitive evidence and guide optimal implementation of wound edge protectors in surgical practice.
CONCLUSION
This retrospective comparative study suggests that the use of wound edge protectors is associated with a reduced risk of surgical site infections (SSIs) in patients undergoing open appendectomy for acute appendicitis. In addition to lowering SSI rates, the use of wound edge protectors was linked to improved perioperative outcomes, including reduced blood loss, lower post-operative pain, and shorter hospital stays. However, given the observational design and potential for residual confounding, these findings should be interpreted with caution. Further high-quality, multicentre randomised controlled trials are warranted to validate these results and guide best practices in SSI prevention.
Acknowledgments
The authors would like to extend their sincere gratitude Department of Surgery, Faculty of Medicine Vajira Hospital, Navamindradhiraj University, for facilitating this study. Finally, we express our appreciation to the patients and medical staff whose participation and cooperation made this research possible.
Conflict of Interest
The authors declare no conflicts of interest.
Funding Source
This study was funded by a grant from the Faculty of Medicine Vajira Hospital, Navamindradhiraj University.
REFERENCE
1. Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278-87.
2. Moris D, Paulson EK, Pappas TN. Diagnosis and Management of Acute Appendicitis in Adults: A Review. Jama. 2021;326(22): 2299-311.
3. Borruel Nacenta S, Ibáñez Sanz L, Sanz Lucas R, Depetris MA, Martínez Chamorro E. Update on acute appendicitis: Typical and untypical findings. Radiologia (Engl Ed). 2023;65 Suppl 1:S81-s91.
4. Gouda NS. Surgical Site Infection. Journal of Pioneering Medical Sciences. 2025;14:21-33.
5. Azoury SC, Farrow NE, Hu QL, Soares KC, Hicks CW, Azar F, et al. Postoperative abdominal wound infection–epidemiology, risk factors, identification, and management. Chronic Wound Care Management and Research. 2015:137-48.
6. Ortega G, Rhee DS, Papandria DJ, Yang J, Ibrahim AM, Shore AD, et al. An evaluation of surgical site infections by wound classification system using the ACS-NSQIP. J Surg Res. 2012;174(1):33-8.
7. Yang L, Zheng R, Li H, Ren Y, Chen H. The burden of appendicitis and surgical site infection of appendectomy worldwide. J Infect Dev Ctries. 2023;17(3):367-73.
8. Lohsiriwat V, Chinswangwatanakul V, Lohsiriwat D, Rongrungruang Y, Malathum K, Ratanachai P, et al. Guidelines for the prevention of surgical site infection: the surgical infection society of Thailand recommendations. 2020.
9. De Simone B, Sartelli M, Coccolini F, Ball CG, Brambillasca P, Chiarugi M, et al. Intraoperative surgical site infection control and prevention: a position paper and future addendum to WSES intra-abdominal infections guidelines. World J Emerg Surg. 2020; 15(1):10.
10. De Pastena M, Marchegiani G, Paiella S, Fontana M, Esposito A, Casetti L, et al. Use of an intraoperative wound protector to prevent surgical-site infection after pancreatoduodenectomy: randomized clinical trial. Br J Surg. 2020;107(9):1107-13.
11. Ahmed K, Connelly TM, Bashar K, Walsh SR. Are wound ring protectors effective in reducing surgical site infection post appendectomy? A systematic review and meta-analysis. Ir J Med Sci. 2016; 185(1):35-42.
12. Kobayashi H, Uetake H, Yasuno M, Sugihara K. Effectiveness of Wound-Edge Protectors for Preventing Surgical Site Infections after Open Surgery for Colorectal Disease: A Prospective Cohort Study with Two Parallel Study Groups. Dig Surg. 2019;36(1):83-8.
13. Zhang L, Elsolh B, Patel SV. Wound protectors in reducing surgical site infections in lower gastrointestinal surgery: an updated meta-analysis. Surg Endosc. 2018;32(3):1111-22.
14. Edwards JP, Ho AL, Tee MC, Dixon E, Ball CG. Wound protectors reduce surgical site infection: a meta-analysis of randomized controlled trials. Ann Surg. 2012;256(1):53-9.
15. Mihaljevic AL, Müller TC, Kehl V, Friess H, Kleeff J. Wound edge protectors in open abdominal surgery to reduce surgical site infections: a systematic review and meta-analysis. PLoS One. 2015;10(3): e0121187.
16. Itatsu K, Yokoyama Y, Sugawara G, Kamiya S, Terasaki M, Morioka A, et al. The Benefits of a Wound Protector in Preventing Incisional Surgical Site Infection in Elective Open Digestive Surgery: A Large-Scale Cohort Study. World J Surg. 2017;41(11):2715-22.
17. Humes DJ, Simpson J. Acute appendicitis. Bmj. 2006;333(7567): 530-4.
18. Mihaljevic AL, Schirren R, Özer M, Ottl S, Grün S, Michalski CW, et al. Multicenter double-blinded randomized controlled trial of standard abdominal wound edge protection with surgical dressings versus coverage with a sterile circular polyethylene drape for prevention of surgical site infections: a CHIR-Net trial (BaFO; NCT01181206). Ann Surg. 2014;260(5):730-7; discussion 7-9.
19. Horiuchi T, Tanishima H, Tamagawa K, Matsuura I, Nakai H, Shouno Y, et al. Randomized, controlled investigation of the anti-infective properties of the Alexis retractor/protector of incision sites. J Trauma. 2007;62(1):212-5.
Full Text Sources:
Abstract:
Views: 18

For Authors
Journal Subscriptions

Sept 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News