Surgery, Gastroenterology and Oncology
Official journal of the International Association of Surgeons, Gastroenterologists and Oncologists
|
|
Evaluation of Mesh Reinforcement during Intestinal Stoma Closure in Prevention of Stomal Site Incisional Hernia: Randomized Controlled Trial
Background: Incisional hernia is an undervalued complication after stoma closure, with rates
about 40%. Mesh-reinforced stoma reversal might be a simple and applicable approach to
decrease the frequency of incisional hernia. There is a current debate about efficacy of this
technique in preventing incisional hernias following stoma closure.
Methods: In this prospective clinical study, all patients with temporary stoma who admitted to Mansoura University Hospital at the period from February 2019 to April 2021 and fulfill the eligibility criteria were distributed into 2 groups. In group I conventional sutured fascial closure was done while in group-II mesh reinforced fascial closure was done during stoma reversal.
Results: Time to stoma closure had mean values of 26.76 and 24 weeks in Groups 1 and 2 respectively (p = 0.430). Surgical site infections (SSI) were encountered in 20% and 19% of patients in the two groups (p = 0.868). The occurrence of stoma site incisional hernia (SSIH) showed a significant increase in Group 1 (20% vs 2% in the other group – p = 0.009).
Conclusion: prophylactic mesh reinforcement throughout stoma closure significantly reduces the incidence of stoma site incisional hernia with no significant increase in the incidence of the stoma site wound infection.
INTRODUCTION
The expression "Stoma" refers to formation of an artificial hole into a hollow organ to be exteriorized on the body surface (1). In 1776, Pillore created the first reported stoma. Within gastro-intestinal operations, stomas were frequently fashioned as a colostomy or ileostomy (2). These might be temporary or permanent and might be created from the bowel ending or the side of the bowel still in continuity (named as a loop stoma) (3).
Temporary stomas are made to divert intestinal content away from a distal anastomosis or obstructing lesion, before a second surgery to reestablish bowel continuousness. In addition they can be a substitute to primary anastomosis in emergency surgery in patients with bad general condition whose primary anastomosis is unsafe (4). The European Hernia Society defines incisional hernia as defects in the abdominal wall that either contain or are free of a bulge surrounding postoperative scars. They can be seen or palpated clinically or radiologically identified (5).
Post-operative incisional hernias are associated with multiple morbidities affecting quality of life (QoL) of patients and imposing economical burden on health care system. Lethal complications as strangulation or incarceration could occur necessitating urgent interventions (6,7,8).
The development of incisional hernias could be contributed to either patient related or operative factors (9).
Mesh-reinforced stoma reversal considered a simple and practical approach to decrease the possible incidence of incisional hernias. In spite of various reports validated the usage of prosthetic mesh for incisional hernias repairing (10), there is a current debate about its efficacy in preventing incisional hernias development following stoma reversal. Sensibly, many physicians are doubtful to place prosthetic mesh in potentially contaminated wounds given the lack of information and fear of wounds complications, fistula establishment which may necessitate mesh extraction or long-term anti-biotic therapy (11). On the other hand, latest reports advocate that these side-effects might be clarified in great portion by technical errors in mesh placement more than wounds contaminations (12). With advanced mesh technologies and operative approaches, it might be probable to decrease the frequency of SSIH with no cumulative wounds' complications.
In the current work we are aiming to assess the role of mesh-reinforced stoma closure in decreasing the risk of developing SSIH without increasing the risk of surgical site infection and to identify responsible risk factors for incisional hernia development after stoma closure.
PATIENTS AND METHODS
In this prospective clinical study, all cases with temporary stoma who admitted to Mansoura University Hospital at the period from February 2019 to April 2021 and fulfill the criteria of eligibility were included. Informed written consent was taken from all cases before being enrolled in this work. The study population was randomly distributed into 2 groups: Group I: Patients with temporary stoma in which conventional sutured fascial closure was done during stoma reversal. Group-II: Patients with temporary stoma in which mesh reinforced fascial closure was done during stoma reversal.
Method of randomization
Cases were arbitrarily allocated into 2 groups; Group-I (conventional closure) and group-II (meshreinforced closure). Simple randomization with 1:1 allocation ratio has been done by means of online arbitrary number generating package (www.randomization.com). Arbitrarily produced treatments distributions have been putted in sealed envelopes. After the case get the anesthesia, the envelope was opened in the surgical room by the circulating nurses and the case was then assigned to one of the two treatment groups. This work was dual-blinded as neither the cases, nor the outcome evaluators throughout following-up were knowledgeable of the group to which the case was allocated. The surgeons were knowledgeable of the nature of the research and group distributions.
Sample size calculation
The needed sample-size has been determined by means of the IBMa-SPSSa Sample-Powera v-3.0.1 (IBMa, USA). According to intensive literature review, the incidence of postoperative incisional hernia in the group of cases with mesh reinforcement, in the study conducted by Liu et al. (2013) was 6.4% in the omentopexy group and 36.1% patients without mesh reinforcement. Entire number of 84 cases (42 in every group) was calculated to detect an expected difference of 10% change in the overall frequency of postoperative incisional hernia at 95% level of significance and power of 80%.
Inclusion criteria
Patients aged above 18, patients with temporary double barreled and simple loop ostomy, patients with American Society of anesthesiologists (ASA) physical status sorting 1&2.
Exclusion criteria
Patients with anastomotic leak after closure that necessitates re-exteriorization of the bowel, patients with midline incisional hernia from the previous surgery, patients with end ostomy or Hartman’s colostomy that need laparotomy for closure, patients with permanent stoma, patients with ASA physical status classification > 2 and patients not willing to participate in the study.
Operative technique
Stoma reversal in both groups was carried out by the same technique as follow: performing an opening in the skin surrounding the stoma 3–4 mm from the muco-cutaneous junctions. Separate the bowel loop away from its attachment to the abdomen wall. Cut out a rim of 0.3–0.4 cm of scarred bowel edges exposes healthful tissue.

Closing of bowel defect can be made by double layer of 3-0 vicryl interrupted Suture or stapling by triangulations with 2 applications of the 55 mm linear-stapler in transverse fashion. Once the tissue is of poor quality for simply closing, we expand the incision in the abdomen wall and resect a section. An end-to-end anastomosis is created using the conventional 2-layers suture method or the staple technique. Lastly, irrigation the surgical field and reduction of the bowel into the abdomen are carried out.
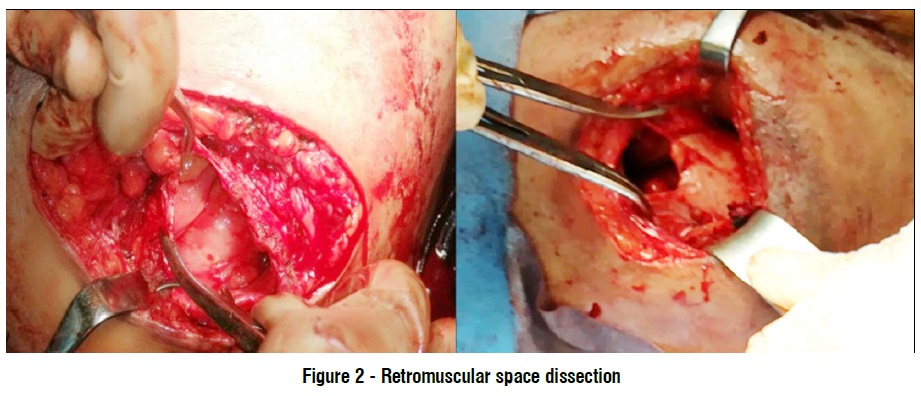
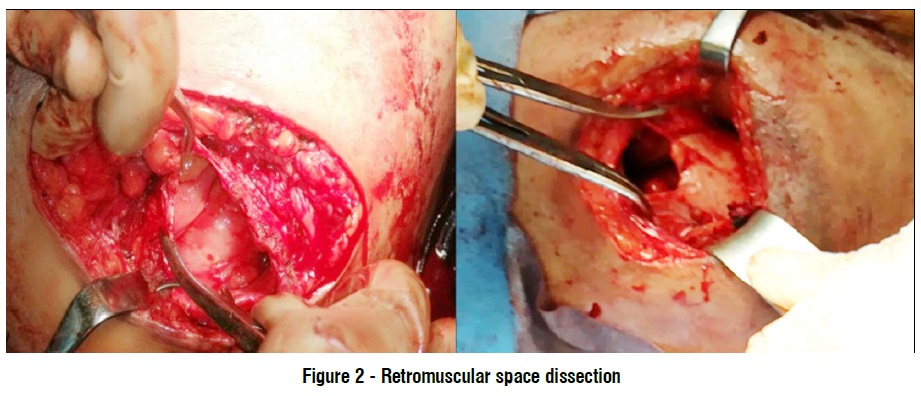
Fascial closure: Group-I: irrigating the surgical field with a dilute anti-biotics and use an Allis clamp to grip the mid-point of the abdomen wall on the lower and upper edges of the defect. Then closes the opening by continuous sutures using nylon loop size 1 (fig. 1). Group-II: Abdominal wall closure was reinforced by retromuscular mesh by the following technique: Dissection through the plane amid the posterior rectus sheath and rectus muscles until the posterior sheath has been completely mobilized. Then closure of the fascial defect of the posterior rectus sheath. A piece of non-absorbable macroporus polyproprylene mesh (ParieteneTM mesh by COVIDENTM) with mesh coverage of 5 cm beyond defect size (15×15 in most of cases) is placed amid the posterior rectus sheath and the rectus muscles and fixated to the muscle layer above with four trans-fascial polypropelene sutures in the four angles of the mesh. Then closure of the anterior rectus sheath by continuous suturing using nylon loop size 1 (fig. 2, 3).
Postoperative care and follow up
Standard post-operative care, including mobilization and fast restoration of ordinary diet. Systemic anti-biotics aren’t given beyond the peri-operative interval except if there were severe wound contamination throughout the operation. Postoperative evaluation of early complications as SSI, anastomotic leak and wound dehiscence are done on regular weekly visits for one month. Long-term follow up visits at 3, 6 and 9 months are done to detect stoma site incisional hernia development or fistula formation. Both early and long term evaluations are done by clinical examination and radiological assessment when clinical findings are non-conclusive.

Statistical analysis of the data: collected data analyzed using IBM SPSS-27 program. Qualitative data have been presented as numbers and percent. Quantitative have been presented as median (min and max) for non-parametric data and mean, SD for parametric data thereafter examining normality by means of Kolmogrov-Smirnov testing. Results was Significant at p<0.05.
Data analysis
Qualitative data: Chi-Square testing used to compare 2 or more groups. Monte Carlo test as correction for Chi-Square testing when >25% of cells have count <5 in tables (>2*2). Fischer Exact test has been utilized as correction for Chi-Square test when >25% of cells have count <5 in 2*2 tables. Quantitative data between two groups: Parametric test: Student t-test has been utilized for comparing 2 non-dependent variables. Non-Parametric test: Mann-Whitney U test has been utilized for comparing 2 non-dependent variables. Wilcoxon signed rank test: has been utilized for comparing 2 non-dependent variables. Uni-variate and multi-variate logistic regressions analysis has been used to assess the associations among dependent and independent risk predictors of a binary categorical outcome. Level of significance: results were nonsignificant if the p > 0.05, Significant at p ? 0.05 and highly significant at p < 0.001.
RESULTS
Starting with demographics, the ages mean of the enrolled patients was 52 and 53.56-yrs in groups 1and 2 respectively. Males represented 56% and 54% of patients in the same groups respectively, whereas the remaining cases were females. In addition, BMI had mean values of 34.67 and 35.51 kg/m2 in the same two groups respectively. All of the previous parameters were non significantly differed between the study groups (p value > 0.05). The prevalence of systemic comorbidities showed no significant difference between the two study groups (p > 0.05). Chronic liver disease (CLD) was present in 7% and 9% of patients, whereas diabetes (DM) was present in 31% and 23% of cases in the same 2 groups respectively. Time to stoma closure had mean values of 26.76 and 24 weeks in Groups 1 and 2 respectively, with nonsignificant difference among the study groups (p value= 0.430) table 1.


The indication of primary operation and stoma were non-significantly differed among the study groups (p = 0.817). Colon cancer was the most common indication, followed by mesenteric vascular occlusion (MVO) and volvulus. Other indications included inflammatory bowel disease (IBD), trauma and diverticulosis. The type of stoma also non-significantly differed among the study groups (p value= 0.786), as ileostomy was performed in 53% and 51% of patients in Groups 1 and 2 respectively. However, operative time showed a significant increase in group 2 (84.65 vs. 51.56 minutes in group 1 – p < 0.001). The method of anastomotic creation was also comparable between the study groups (p = 0.191), as hand sewn anastomosis was done in 51% and 47% of patients in the same two groups respectively, while the remaining cases were performed via stapler (table 2).
The duration of hospitalization was non-significantly differed among the study groups (p = 0.991), as it had mean values of 5.89 and 5.88 days in Groups 1 and 2 both groups (p value = 0.657), as it had mean values of 10.4 and 10.09 days in the same groups respectively (table 3).
Surgical site infection (SSI) was encountered in 20% and 19% of patients in the same two groups, with nonsignificant difference among them (p value= 0.868). The incidence of stoma site incisional hernia (SSIH) showed a significant increase in Group 1 (20% vs 2% in the other group – p = 0.009). Leakage was encountered in only one case in each group, with no significant difference on statistical analysis (table 4).
We encountered 9 cases of SSI in the first group, 6 of them were superficial infections that were treated conservatively by culture & sensitivity with antibiotic therapy, the other 3 cases had deep wound infections that were treated by open wound drainage, irrigation, antibiotic therapy and secondary wound closure after improvement. While in the second group 8 cases had SSI, 4 of them were superficial infections that were treated conservatively by the same measures as the first group. The other 4 cases had deep wound infection, 3 of them improved by open drainage irrigation and antibiotic therapy. One case with deep retromuscular collection needed US guided drainage and antibiotic therapy. Meshes were preserved in all cases (table 5). The presence of ileostomy was a risk-factor for SSI on univariate analysis. However, this factor showed no significance on multivariate analysis. No other parameters showed to be a significantly associated riskfactor for that complication (table 6).
On univariate analysis, BMI, operative time, diabetes, colon cancer and SSI were significant risk-factors for SSIH (p < 0.05). While both colon cancer and SSI maintained their significance on multivariate analysis (table 7).
DISCUSSION
Up to 48 percent of cases with a stoma face complication, like high output, prolapse, retraction, or parastomal hernias, resulting in skin irritation, pains, complications with stoma bag applications, restrictions on physical activities, aesthetic complaint, and decreased QoL (13).



The optimum way for solving those complications is reversal of the stoma, which was done in about 66% of temporary stomas (14). Though, stoma reversal carries frequently undervalued rate of morbidities and mortalities, with complications such as post-operative bowel obstructions, wound infections, and anastomotic leak, happening in 20- 27% of cases (15). The current study was conducted at Mansoura University Hospitals aiming to investigate effectiveness and safety of prophylactic mesh placement in preventions of SSIH. We included a total of 88 patients who were allocated to 2 groups; Group 1 comprised 45 cases who experienced stomal site closure without mesh, and Group 2 included the remaining 43 patients who had mesh reinforcement. The mean age of the comprised patients showed nonsignificant difference among the study groups.
In a similar report handling the same perspective, Warren et al. reported that the included patients had mean age of 57.3 and 54.8 years in the mesh group and controls resp., with nonsignificant difference among the study groups (p = 0.09) (16).
Although Liu et al. reported older age range compared to ours (69.6 and 65 years in the mesh group and controls resp.), statistical analysis showed nonsignificant difference among the study groups (p = 0.301) (17). Both of the previous studies agreed with our findings.
In our study, BMI was comparable among the study groups.
Pizza et al. reported comparable BMI between cases in the mesh group and controls (p > 0.05). It had mean values of 24 and 23 kg/m2 in the same groups respectively (18).
In contrast, Warren et al. revealed significantly higher BMI in the mesh than controls (p = 0.001). BMI had mean values of 30.2 and 27.3 kg/m2 in the same groups respectively (16).
In our study, the interval throughout which stomas still in situ was about 6-mths in the two study groups, which is comparable to other studies (15). In the present work, operative time showed a significantly longer in group 2. Of course, this time was needed for mesh installation and fixation, which was omitted in Group 1.
In the same context, Warren and his coworkers reported a significant prolongation of operative time in association with mesh installation (p < 0.001). It had mean values of 255 and 133.5 minutes in the mesh group and controls respectively (16). It is reasonable to find some differences between different studies regarding operative time, which depend on surgical experience, stoma type (end versus loop) and available healthcare facilities.
In the current study, the duration of hospitalization showed nonsignificant difference among the study groups.
Another study reported that the period of hospitalization was comparable among the mesh group and controls (p = 0.534), as is it had a median value of 5 days in both groups (17).
In the current study, SSI showed nonsignificant difference between the two study groups. Likewise, Warren et al. reported that SSI was detected in 20% and 19.8% of patients in the mesh group and controls respectively, with nonsignificant change among the study groups (p = 1) (16).
Other authors reported nonsignificant difference among the study groups regarding post-operative SSI rates (p = 1), which was encountered in 4.3% and 2.8% of patients in the mesh group and controls resp. (17). Risk of SSI in mesh group could be reduced by using slowly resorbable meshes for fascial reinforcement (PHASIX TM mesh) due its safety in potential contaminated surgical fields as claimed by van Rooijen and his colleagues, but this technique needs further evaluation in upcoming studies (19).
When it comes to our primary outcome, the incidence of incisional hernia showed a significant increase in Group 1. It was evident that mesh placement is protective against that complication.
Randomized trials have validated that mesh application reduces recurrences of incisional hernias (20); consequently, prophylactic mesh application was supported by some reports for reinforcing the fascia repairs post stoma reversal (17).
In our study, leakage was encountered in only one case in each group, with no significant difference on statistical analysis.
Likewise, Liu and his colleagues reported that the incidence of post-operative intraabdominal septic complications was comparable between the two groups (p = 1). It was encountered in 4.3% and 5.6% of patients in the mesh group and controls respectively (17). Another study negated the occurrence of leakage in the mesh group while it was encountered in two cases in the control group (3%). Nevertheless, no significant difference was detected on statistical analysis (p = 0.328) (21).
In the recent study conducted by Pizza and his colleagues, anastomotic leakage was detected in 0% and 1.7% of patients in the mesh group and controls resp. (p > 0.05) (18). Another study confirmed the previous findings regarding comparable incidence of anastomotic leakage between mesh group and controls (p = 0.25) (16).
When it comes for risk-factors for incisional hernia after stomal closures in our work, high BMI was a significant risk-factor for the same complication on univariate analysis. The obesity-persuaded straight force that raises abdomen wall tension secondary to high intra-abdomen pressure can clarify why obesity is a risk-factor for incisional hernias (22). The inherent anatomic characteristics of adipose tissue, vascular deficiency, cellular and composition modification, oxidative stress, changes in immune intermediaries, and nutritious shortages can as well negatively impact wound healing (23).
In line with our findings, Schreinemacher and his associates reported that high BMI was a significant risk-factor for incisional hernia subsequent to stomal closure (p = 0.02). Incisional hernia was encountered in 25.8% of patients in patients with BMI < 30 kg/m2, whereas the same complication occurred in 59.1% of patients with higher BMI (24). On the other hand, Liu et al. denied any significant impact of BMI on the development of this complication (p = 0.977). It had mean values of 26.1 and 26.7 kg/m2 in the hernia and nonhernia groups respectively (17).
Our findings showed that diabetes is a significant risk-factor for incisional hernia on univariate analysis. We think that chronic micro-vascular variations secondary to DM damages tissue perfusions, decreasing the influx of inflammatory cells and compounds to the wound location, causing poor collagen depositions and a tendency for wound dehiscence (25).
Another study confirmed our findings, as diabetes showed significantly higher prevalence in the hernia versus the non-hernia groups (11.2% vs. 6.4% - p = 0.03) (26). However, another study negated any significant impact of diabetes on the development of the same complication (p = 0.343) (27).
In our study, the type of stoma wasn't a significant risk-factor for incisional hernia following stoma closure. Schreinemacher et al. reported that the type of stoma did not have a significant impact on the development of that complication (p = 0.92) (24). However, another study found that loop colostomy was a significant predictor for incisional hernia after closure (HR = 2.12) (26). Our findings showed that colon cancer was a significant predictor for incisional hernia after stoma reversal on both univariate and multivariate analyses. This could be explained by the fact that malignancy causes mal-nutrition and poor general health, which is combined by the immuno-suppressive impacts of chemo-therapy (28). Another study reported that malignancy is a significant risk-factor for incisional hernia after stomal reversal (p = 0.032). Patients with malignant indication constituted 93.8% and 71.6% of patients in the hernia and non-hernia groups respectively (17). Contrarily, Sharp and his colleagues denied any significant impact of cancer colon on the advance of incisional hernia after stomal closure (p = 0.32). Colon cancer was the primary indication of surgery in 23.5% and 27.6% of patients in the hernia and nonhernia groups respectively (26).
Our findings showed that SSI was a significant predictor for incisional hernia after stoma reversal on both univariate and multivariate analyses. Walming and his associates confirmed our findings as the presence of surgical site infection was a significant predictor for wound dehiscence (CI 1.65–5.46 - p < 0.001) and incisional hernia (CI 2.38–5.71 - p < 0.001) (29). Several reports also confirmed our perspectives (28, 30).
On the other hand, Niggebrugge et al. could not find such a relationship (31).
Surgical site infection induces abnormal collagen metabolism, and inhibits and delays the fascial woundhealing process, especially in the proliferative phase, leading to an increased risk of incisional hernia (32). In the current study, long operative time appeared to be a significant risk-factor for incisional hernia after stomal reversal on univariate analysis. To our knowledge, no preceding study had made this correlation, and we could explain it by the fact that long operative time could be an indicator for other parameters like obesity, which could increase herniation rates. This parameter needs to be furtherly investigated in future studies.
Our findings showed that the existence of ileostomy was a risk-factor for surgical site infection on univariate analysis. No other parameters showed to be a significant risk-factor for that complication. Perhaps soiling and watery content of the ileostomy could potentiate that problem.
In another study, authors agreed with our findings as age, BMI, diabetes, and smoking did not have a negative impact on the development of surgical site infection after closure. Although authors did not report ileostomy as a risk-factor, linear incision closure was a significant risk-factor for that complication (p = 0.007) (33). Our work has some limitations, as it is a single center report that comprised a comparatively small sample size. This drawback should be well-covered in the upcoming studies.
CONCLUSION
Prophylactic mesh reinforcement during stoma reversal significantly decreases the incidence of stoma site incisional hernia without significant increase in the incidence of the stoma site wound infection.
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
For this study was approval from the institutional review board was obtained. IRB registration code: MD.19.01.136. Informed written consent: was taken from all cases before being enrolled in this work.
REFERENCES
1. Harries R, Torkington J. Stomal closure: strategies to prevent incisional hernia. Frontiers in surgery. 2018;5:28. eCollection 2018.
2. Memon Z, Qureshi S, Hakeem A. Outcome of closure of transient ileostomy at tertiary care hospital. In Med. Forum. 2019; 30(6): 123.
3. Cingi A, Cakir T, Sever A, Aktan A. Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum. 2006;49(10):1559-63
4. Pine J, Stevenson, L. Intestinal stomas. Surgery (Oxford). 2017; 35(3):165-170.
5. Muysoms F, Miserez M, Berrevoet F, Campanelli G, Champault G, Chelala E, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13(4):407-414.
6. van Ramshorst G, Eker H, Hop W, Jeekel J, Lange J. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012;204(2):144-50.
7. Kassem M, El-Haddad H. Polypropylene-based composite mesh versus standard polypropylene mesh in the reconstruction of complicated large abdominal wall hernias: a prospective randomized study. Hernia. 2016;20(5):691-700.
8. Sandy-Hodgetts K, Leslie G, Lewin G, Hendrie D, Carville K. Surgical wound dehiscence in an Australian community nursing service: time and cost to healing. J Wound Care. 2016;25(7):377-83.
9. Adell-Carceller R, Segarra-Soria M, Pellicer-Castell V, Marcote- Valdivieso E, Gamón-Giner R, Martin-Franco M, et al. Incisional hernia in colorectal cancer surgery. Associated risk-factors. Cir Esp. 2006;79(1):42-5.
10. Porrero J, Cano-Valderrama O, Castillo M, Marcos A, Tejerina G, Cendrero M, et al. Importance of mesh overlap on hernia recurrence after open umbilical hernia repair with bilayer prosthesis. Am J Surg. 2018;216(5):919-922.
11. Herbert G, Tausch T, Carter P. Prophylactic mesh to prevent incisional hernia: a note of caution. Am J Surg. 2009;197(5):595- 8; discussion 598
12. López-Cano M, Brandsma H, Bury K, Hansson B, Kyle-Leinhase I, Alamino J, et al. Prophylactic mesh to prevent parastomal hernia after end colostomy: a meta-analysis and trial sequential analysis. Hernia. 2017;21(2):177-189.
13. Krishnamurty, D, Blatnik, J, Mutch, M. Stoma complications. Clin Colon Rectal Surg. 2017;30(3):193-200.
14. Sier, M, Van Gelder, L, Ubbink, D, Bemelman, W, Oostenbroek, R. Factors affecting timing of closure and non-reversal of temporary ileostomies. Int J Colorectal Dis. 2015;30(9):1185-92.
15. Schreinemacher, M, Vijgen, G, Dagnelie, P, Bloemen, J, Huizinga, B, Bouvy, NIncisional hernias in temporary stoma wounds: a cohort study. Arch Surg. 2011;146(1):94-9.
16. Warren, J, Beffa, L, Carbonell, A, Cull, J, Sinopoli, B, Ewing, J, et al. Prophylactic placement of permanent synthetic mesh at the time of ostomy closure prevens formation of incisional hernias. Surgery. 2018;163(4):839-846.
17. Liu D, Banham E, Yellapu S. Prophylactic mesh reinforcement reduces stomal site incisional hernia after ileostomy closure. World J Surg. 2013;37(9):2039-45.
18. Pizza F, D’Antonio D, Arcopinto M, Dell’Isola C, Marvaso A. Safety and efficacy of prophylactic resorbable biosynthetic mesh in loopileostomy reversal: a case–control study. Updates Surg. 2020;72(1): 103-108
19. van Rooijen MM, Jairam AP, Tollens T, Jørgensen LN, de Vries Reilingh TS, Piessen G, et al. Outcomes of a new slowly resorbable biosynthetic mesh (Phasix®) in potentially contaminated incisional hernias: A prospective, multi-center, single-arm trial. Int J Surg. 2020;83:31-36.
20. Luijendijk R, Hop W, Van Den Tol M, De Lange D, Braaksma M, IJzermans J, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343(6):392-8.
21. Maggiori L, Moszkowicz D, Zappa M, Mongin C, Panis Y. Bioprosthetic mesh reinforcement during temporary stoma closure decreases the rate of incisional hernia: a blinded, case-matched study in 94 patients with rectal cancer. Surgery. 2015;158(6):1651-7
22. Lambert D, Marceau S, Forse R. Intra-abdominal pressure in the morbidly obese. Obes Surg. 2005;15(9):1225-32.
23. Pierpont Y, Dinh T, Salas R, Johnson E, Wright T, Robson M, et al. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936. eCollection 2014.
24. Schreinemacher M, Vijgen G, Dagnelie P, Bloemen J, Huizinga B, Bouvy N. Incisional hernias in temporary stoma wounds: a cohort study. Arch Surg. 2011;146(1):94-9.
25. van Ramshorst G, Nieuwenhuizen J, Hop W, Arends P, Boom J, Jeekel J, et al. Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg. 2010;34(1):20-7.
26. Sharp S, Francis J, Valerian B, Canete J, Chismark A, Lee E. Incidence of ostomy site incisional hernias after stoma closure. Am Surg. 2015;81(12):1244-8.
27. Lorenz A, Kogler P, Kafka-Ritsch R, Öfner D, Perathoner A. Incisional hernia at the site of stoma reversal - incidence and risk-factors in a retrospective observational analysis. Int J Colorectal Dis. 2019; 34(7):1179-1187.
28. Riou J, Cohen J, Johnson Jr H. Factors influencing wound dehiscence. Am J Surg. 1992;163(3):324-30.
29. Walming S, Angenete E, Block M, Bock D, Gessler B, Haglind E. Retrospective review of risk factors for surgical wound dehiscence and incisional hernia. BMC Surg. 2017;17(1):19.
30. Gislason H, Søreide O, Viste A. Wound complications after major gastrointestinal operations. The surgeon as a risk factor. Dig Surg. 1999;16(6):512-4.
31. Niggebrugge AH, Trimbos JB, Hermans J, Steup WH, Van De Velde CJ. Influence of abdominal-wound closure technique on complications after surgery: a randomised study. Lancet. 1999;353(9164): 1563-7.
32. Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 2014;101(11):1439-47.
33. Yamamoto M, Tanaka K, Masubuchi S, Ishii M, Hamamoto H, Suzuki S, et al. Risk-factors for surgical site infection after stoma closure comparison between pursestring wound closure and conventional linear wound closure: propensity score matching analysis. Am J Surg. 2018;215(1):58-61.
Full Text Sources:
Abstract:
Views: 2715

Methods: In this prospective clinical study, all patients with temporary stoma who admitted to Mansoura University Hospital at the period from February 2019 to April 2021 and fulfill the eligibility criteria were distributed into 2 groups. In group I conventional sutured fascial closure was done while in group-II mesh reinforced fascial closure was done during stoma reversal.
Results: Time to stoma closure had mean values of 26.76 and 24 weeks in Groups 1 and 2 respectively (p = 0.430). Surgical site infections (SSI) were encountered in 20% and 19% of patients in the two groups (p = 0.868). The occurrence of stoma site incisional hernia (SSIH) showed a significant increase in Group 1 (20% vs 2% in the other group – p = 0.009).
Conclusion: prophylactic mesh reinforcement throughout stoma closure significantly reduces the incidence of stoma site incisional hernia with no significant increase in the incidence of the stoma site wound infection.
INTRODUCTION
The expression "Stoma" refers to formation of an artificial hole into a hollow organ to be exteriorized on the body surface (1). In 1776, Pillore created the first reported stoma. Within gastro-intestinal operations, stomas were frequently fashioned as a colostomy or ileostomy (2). These might be temporary or permanent and might be created from the bowel ending or the side of the bowel still in continuity (named as a loop stoma) (3).
Temporary stomas are made to divert intestinal content away from a distal anastomosis or obstructing lesion, before a second surgery to reestablish bowel continuousness. In addition they can be a substitute to primary anastomosis in emergency surgery in patients with bad general condition whose primary anastomosis is unsafe (4). The European Hernia Society defines incisional hernia as defects in the abdominal wall that either contain or are free of a bulge surrounding postoperative scars. They can be seen or palpated clinically or radiologically identified (5).
Post-operative incisional hernias are associated with multiple morbidities affecting quality of life (QoL) of patients and imposing economical burden on health care system. Lethal complications as strangulation or incarceration could occur necessitating urgent interventions (6,7,8).
The development of incisional hernias could be contributed to either patient related or operative factors (9).
Mesh-reinforced stoma reversal considered a simple and practical approach to decrease the possible incidence of incisional hernias. In spite of various reports validated the usage of prosthetic mesh for incisional hernias repairing (10), there is a current debate about its efficacy in preventing incisional hernias development following stoma reversal. Sensibly, many physicians are doubtful to place prosthetic mesh in potentially contaminated wounds given the lack of information and fear of wounds complications, fistula establishment which may necessitate mesh extraction or long-term anti-biotic therapy (11). On the other hand, latest reports advocate that these side-effects might be clarified in great portion by technical errors in mesh placement more than wounds contaminations (12). With advanced mesh technologies and operative approaches, it might be probable to decrease the frequency of SSIH with no cumulative wounds' complications.
In the current work we are aiming to assess the role of mesh-reinforced stoma closure in decreasing the risk of developing SSIH without increasing the risk of surgical site infection and to identify responsible risk factors for incisional hernia development after stoma closure.
PATIENTS AND METHODS
In this prospective clinical study, all cases with temporary stoma who admitted to Mansoura University Hospital at the period from February 2019 to April 2021 and fulfill the criteria of eligibility were included. Informed written consent was taken from all cases before being enrolled in this work. The study population was randomly distributed into 2 groups: Group I: Patients with temporary stoma in which conventional sutured fascial closure was done during stoma reversal. Group-II: Patients with temporary stoma in which mesh reinforced fascial closure was done during stoma reversal.
Method of randomization
Cases were arbitrarily allocated into 2 groups; Group-I (conventional closure) and group-II (meshreinforced closure). Simple randomization with 1:1 allocation ratio has been done by means of online arbitrary number generating package (www.randomization.com). Arbitrarily produced treatments distributions have been putted in sealed envelopes. After the case get the anesthesia, the envelope was opened in the surgical room by the circulating nurses and the case was then assigned to one of the two treatment groups. This work was dual-blinded as neither the cases, nor the outcome evaluators throughout following-up were knowledgeable of the group to which the case was allocated. The surgeons were knowledgeable of the nature of the research and group distributions.
Sample size calculation
The needed sample-size has been determined by means of the IBMa-SPSSa Sample-Powera v-3.0.1 (IBMa, USA). According to intensive literature review, the incidence of postoperative incisional hernia in the group of cases with mesh reinforcement, in the study conducted by Liu et al. (2013) was 6.4% in the omentopexy group and 36.1% patients without mesh reinforcement. Entire number of 84 cases (42 in every group) was calculated to detect an expected difference of 10% change in the overall frequency of postoperative incisional hernia at 95% level of significance and power of 80%.
Inclusion criteria
Patients aged above 18, patients with temporary double barreled and simple loop ostomy, patients with American Society of anesthesiologists (ASA) physical status sorting 1&2.
Exclusion criteria
Patients with anastomotic leak after closure that necessitates re-exteriorization of the bowel, patients with midline incisional hernia from the previous surgery, patients with end ostomy or Hartman’s colostomy that need laparotomy for closure, patients with permanent stoma, patients with ASA physical status classification > 2 and patients not willing to participate in the study.
Operative technique
Stoma reversal in both groups was carried out by the same technique as follow: performing an opening in the skin surrounding the stoma 3–4 mm from the muco-cutaneous junctions. Separate the bowel loop away from its attachment to the abdomen wall. Cut out a rim of 0.3–0.4 cm of scarred bowel edges exposes healthful tissue.

Closing of bowel defect can be made by double layer of 3-0 vicryl interrupted Suture or stapling by triangulations with 2 applications of the 55 mm linear-stapler in transverse fashion. Once the tissue is of poor quality for simply closing, we expand the incision in the abdomen wall and resect a section. An end-to-end anastomosis is created using the conventional 2-layers suture method or the staple technique. Lastly, irrigation the surgical field and reduction of the bowel into the abdomen are carried out.
Fascial closure: Group-I: irrigating the surgical field with a dilute anti-biotics and use an Allis clamp to grip the mid-point of the abdomen wall on the lower and upper edges of the defect. Then closes the opening by continuous sutures using nylon loop size 1 (fig. 1). Group-II: Abdominal wall closure was reinforced by retromuscular mesh by the following technique: Dissection through the plane amid the posterior rectus sheath and rectus muscles until the posterior sheath has been completely mobilized. Then closure of the fascial defect of the posterior rectus sheath. A piece of non-absorbable macroporus polyproprylene mesh (ParieteneTM mesh by COVIDENTM) with mesh coverage of 5 cm beyond defect size (15×15 in most of cases) is placed amid the posterior rectus sheath and the rectus muscles and fixated to the muscle layer above with four trans-fascial polypropelene sutures in the four angles of the mesh. Then closure of the anterior rectus sheath by continuous suturing using nylon loop size 1 (fig. 2, 3).
Postoperative care and follow up
Standard post-operative care, including mobilization and fast restoration of ordinary diet. Systemic anti-biotics aren’t given beyond the peri-operative interval except if there were severe wound contamination throughout the operation. Postoperative evaluation of early complications as SSI, anastomotic leak and wound dehiscence are done on regular weekly visits for one month. Long-term follow up visits at 3, 6 and 9 months are done to detect stoma site incisional hernia development or fistula formation. Both early and long term evaluations are done by clinical examination and radiological assessment when clinical findings are non-conclusive.

Statistical analysis of the data: collected data analyzed using IBM SPSS-27 program. Qualitative data have been presented as numbers and percent. Quantitative have been presented as median (min and max) for non-parametric data and mean, SD for parametric data thereafter examining normality by means of Kolmogrov-Smirnov testing. Results was Significant at p<0.05.
Data analysis
Qualitative data: Chi-Square testing used to compare 2 or more groups. Monte Carlo test as correction for Chi-Square testing when >25% of cells have count <5 in tables (>2*2). Fischer Exact test has been utilized as correction for Chi-Square test when >25% of cells have count <5 in 2*2 tables. Quantitative data between two groups: Parametric test: Student t-test has been utilized for comparing 2 non-dependent variables. Non-Parametric test: Mann-Whitney U test has been utilized for comparing 2 non-dependent variables. Wilcoxon signed rank test: has been utilized for comparing 2 non-dependent variables. Uni-variate and multi-variate logistic regressions analysis has been used to assess the associations among dependent and independent risk predictors of a binary categorical outcome. Level of significance: results were nonsignificant if the p > 0.05, Significant at p ? 0.05 and highly significant at p < 0.001.
RESULTS
Starting with demographics, the ages mean of the enrolled patients was 52 and 53.56-yrs in groups 1and 2 respectively. Males represented 56% and 54% of patients in the same groups respectively, whereas the remaining cases were females. In addition, BMI had mean values of 34.67 and 35.51 kg/m2 in the same two groups respectively. All of the previous parameters were non significantly differed between the study groups (p value > 0.05). The prevalence of systemic comorbidities showed no significant difference between the two study groups (p > 0.05). Chronic liver disease (CLD) was present in 7% and 9% of patients, whereas diabetes (DM) was present in 31% and 23% of cases in the same 2 groups respectively. Time to stoma closure had mean values of 26.76 and 24 weeks in Groups 1 and 2 respectively, with nonsignificant difference among the study groups (p value= 0.430) table 1.


The indication of primary operation and stoma were non-significantly differed among the study groups (p = 0.817). Colon cancer was the most common indication, followed by mesenteric vascular occlusion (MVO) and volvulus. Other indications included inflammatory bowel disease (IBD), trauma and diverticulosis. The type of stoma also non-significantly differed among the study groups (p value= 0.786), as ileostomy was performed in 53% and 51% of patients in Groups 1 and 2 respectively. However, operative time showed a significant increase in group 2 (84.65 vs. 51.56 minutes in group 1 – p < 0.001). The method of anastomotic creation was also comparable between the study groups (p = 0.191), as hand sewn anastomosis was done in 51% and 47% of patients in the same two groups respectively, while the remaining cases were performed via stapler (table 2).
The duration of hospitalization was non-significantly differed among the study groups (p = 0.991), as it had mean values of 5.89 and 5.88 days in Groups 1 and 2 both groups (p value = 0.657), as it had mean values of 10.4 and 10.09 days in the same groups respectively (table 3).
Surgical site infection (SSI) was encountered in 20% and 19% of patients in the same two groups, with nonsignificant difference among them (p value= 0.868). The incidence of stoma site incisional hernia (SSIH) showed a significant increase in Group 1 (20% vs 2% in the other group – p = 0.009). Leakage was encountered in only one case in each group, with no significant difference on statistical analysis (table 4).
We encountered 9 cases of SSI in the first group, 6 of them were superficial infections that were treated conservatively by culture & sensitivity with antibiotic therapy, the other 3 cases had deep wound infections that were treated by open wound drainage, irrigation, antibiotic therapy and secondary wound closure after improvement. While in the second group 8 cases had SSI, 4 of them were superficial infections that were treated conservatively by the same measures as the first group. The other 4 cases had deep wound infection, 3 of them improved by open drainage irrigation and antibiotic therapy. One case with deep retromuscular collection needed US guided drainage and antibiotic therapy. Meshes were preserved in all cases (table 5). The presence of ileostomy was a risk-factor for SSI on univariate analysis. However, this factor showed no significance on multivariate analysis. No other parameters showed to be a significantly associated riskfactor for that complication (table 6).
On univariate analysis, BMI, operative time, diabetes, colon cancer and SSI were significant risk-factors for SSIH (p < 0.05). While both colon cancer and SSI maintained their significance on multivariate analysis (table 7).
DISCUSSION
Up to 48 percent of cases with a stoma face complication, like high output, prolapse, retraction, or parastomal hernias, resulting in skin irritation, pains, complications with stoma bag applications, restrictions on physical activities, aesthetic complaint, and decreased QoL (13).



The optimum way for solving those complications is reversal of the stoma, which was done in about 66% of temporary stomas (14). Though, stoma reversal carries frequently undervalued rate of morbidities and mortalities, with complications such as post-operative bowel obstructions, wound infections, and anastomotic leak, happening in 20- 27% of cases (15). The current study was conducted at Mansoura University Hospitals aiming to investigate effectiveness and safety of prophylactic mesh placement in preventions of SSIH. We included a total of 88 patients who were allocated to 2 groups; Group 1 comprised 45 cases who experienced stomal site closure without mesh, and Group 2 included the remaining 43 patients who had mesh reinforcement. The mean age of the comprised patients showed nonsignificant difference among the study groups.
In a similar report handling the same perspective, Warren et al. reported that the included patients had mean age of 57.3 and 54.8 years in the mesh group and controls resp., with nonsignificant difference among the study groups (p = 0.09) (16).
Although Liu et al. reported older age range compared to ours (69.6 and 65 years in the mesh group and controls resp.), statistical analysis showed nonsignificant difference among the study groups (p = 0.301) (17). Both of the previous studies agreed with our findings.
In our study, BMI was comparable among the study groups.
Pizza et al. reported comparable BMI between cases in the mesh group and controls (p > 0.05). It had mean values of 24 and 23 kg/m2 in the same groups respectively (18).
In contrast, Warren et al. revealed significantly higher BMI in the mesh than controls (p = 0.001). BMI had mean values of 30.2 and 27.3 kg/m2 in the same groups respectively (16).
In our study, the interval throughout which stomas still in situ was about 6-mths in the two study groups, which is comparable to other studies (15). In the present work, operative time showed a significantly longer in group 2. Of course, this time was needed for mesh installation and fixation, which was omitted in Group 1.
In the same context, Warren and his coworkers reported a significant prolongation of operative time in association with mesh installation (p < 0.001). It had mean values of 255 and 133.5 minutes in the mesh group and controls respectively (16). It is reasonable to find some differences between different studies regarding operative time, which depend on surgical experience, stoma type (end versus loop) and available healthcare facilities.
In the current study, the duration of hospitalization showed nonsignificant difference among the study groups.
Another study reported that the period of hospitalization was comparable among the mesh group and controls (p = 0.534), as is it had a median value of 5 days in both groups (17).
In the current study, SSI showed nonsignificant difference between the two study groups. Likewise, Warren et al. reported that SSI was detected in 20% and 19.8% of patients in the mesh group and controls respectively, with nonsignificant change among the study groups (p = 1) (16).
Other authors reported nonsignificant difference among the study groups regarding post-operative SSI rates (p = 1), which was encountered in 4.3% and 2.8% of patients in the mesh group and controls resp. (17). Risk of SSI in mesh group could be reduced by using slowly resorbable meshes for fascial reinforcement (PHASIX TM mesh) due its safety in potential contaminated surgical fields as claimed by van Rooijen and his colleagues, but this technique needs further evaluation in upcoming studies (19).
When it comes to our primary outcome, the incidence of incisional hernia showed a significant increase in Group 1. It was evident that mesh placement is protective against that complication.
Randomized trials have validated that mesh application reduces recurrences of incisional hernias (20); consequently, prophylactic mesh application was supported by some reports for reinforcing the fascia repairs post stoma reversal (17).
In our study, leakage was encountered in only one case in each group, with no significant difference on statistical analysis.
Likewise, Liu and his colleagues reported that the incidence of post-operative intraabdominal septic complications was comparable between the two groups (p = 1). It was encountered in 4.3% and 5.6% of patients in the mesh group and controls respectively (17). Another study negated the occurrence of leakage in the mesh group while it was encountered in two cases in the control group (3%). Nevertheless, no significant difference was detected on statistical analysis (p = 0.328) (21).
In the recent study conducted by Pizza and his colleagues, anastomotic leakage was detected in 0% and 1.7% of patients in the mesh group and controls resp. (p > 0.05) (18). Another study confirmed the previous findings regarding comparable incidence of anastomotic leakage between mesh group and controls (p = 0.25) (16).
When it comes for risk-factors for incisional hernia after stomal closures in our work, high BMI was a significant risk-factor for the same complication on univariate analysis. The obesity-persuaded straight force that raises abdomen wall tension secondary to high intra-abdomen pressure can clarify why obesity is a risk-factor for incisional hernias (22). The inherent anatomic characteristics of adipose tissue, vascular deficiency, cellular and composition modification, oxidative stress, changes in immune intermediaries, and nutritious shortages can as well negatively impact wound healing (23).
In line with our findings, Schreinemacher and his associates reported that high BMI was a significant risk-factor for incisional hernia subsequent to stomal closure (p = 0.02). Incisional hernia was encountered in 25.8% of patients in patients with BMI < 30 kg/m2, whereas the same complication occurred in 59.1% of patients with higher BMI (24). On the other hand, Liu et al. denied any significant impact of BMI on the development of this complication (p = 0.977). It had mean values of 26.1 and 26.7 kg/m2 in the hernia and nonhernia groups respectively (17).
Our findings showed that diabetes is a significant risk-factor for incisional hernia on univariate analysis. We think that chronic micro-vascular variations secondary to DM damages tissue perfusions, decreasing the influx of inflammatory cells and compounds to the wound location, causing poor collagen depositions and a tendency for wound dehiscence (25).
Another study confirmed our findings, as diabetes showed significantly higher prevalence in the hernia versus the non-hernia groups (11.2% vs. 6.4% - p = 0.03) (26). However, another study negated any significant impact of diabetes on the development of the same complication (p = 0.343) (27).
In our study, the type of stoma wasn't a significant risk-factor for incisional hernia following stoma closure. Schreinemacher et al. reported that the type of stoma did not have a significant impact on the development of that complication (p = 0.92) (24). However, another study found that loop colostomy was a significant predictor for incisional hernia after closure (HR = 2.12) (26). Our findings showed that colon cancer was a significant predictor for incisional hernia after stoma reversal on both univariate and multivariate analyses. This could be explained by the fact that malignancy causes mal-nutrition and poor general health, which is combined by the immuno-suppressive impacts of chemo-therapy (28). Another study reported that malignancy is a significant risk-factor for incisional hernia after stomal reversal (p = 0.032). Patients with malignant indication constituted 93.8% and 71.6% of patients in the hernia and non-hernia groups respectively (17). Contrarily, Sharp and his colleagues denied any significant impact of cancer colon on the advance of incisional hernia after stomal closure (p = 0.32). Colon cancer was the primary indication of surgery in 23.5% and 27.6% of patients in the hernia and nonhernia groups respectively (26).
Our findings showed that SSI was a significant predictor for incisional hernia after stoma reversal on both univariate and multivariate analyses. Walming and his associates confirmed our findings as the presence of surgical site infection was a significant predictor for wound dehiscence (CI 1.65–5.46 - p < 0.001) and incisional hernia (CI 2.38–5.71 - p < 0.001) (29). Several reports also confirmed our perspectives (28, 30).
On the other hand, Niggebrugge et al. could not find such a relationship (31).
Surgical site infection induces abnormal collagen metabolism, and inhibits and delays the fascial woundhealing process, especially in the proliferative phase, leading to an increased risk of incisional hernia (32). In the current study, long operative time appeared to be a significant risk-factor for incisional hernia after stomal reversal on univariate analysis. To our knowledge, no preceding study had made this correlation, and we could explain it by the fact that long operative time could be an indicator for other parameters like obesity, which could increase herniation rates. This parameter needs to be furtherly investigated in future studies.
Our findings showed that the existence of ileostomy was a risk-factor for surgical site infection on univariate analysis. No other parameters showed to be a significant risk-factor for that complication. Perhaps soiling and watery content of the ileostomy could potentiate that problem.
In another study, authors agreed with our findings as age, BMI, diabetes, and smoking did not have a negative impact on the development of surgical site infection after closure. Although authors did not report ileostomy as a risk-factor, linear incision closure was a significant risk-factor for that complication (p = 0.007) (33). Our work has some limitations, as it is a single center report that comprised a comparatively small sample size. This drawback should be well-covered in the upcoming studies.
CONCLUSION
Prophylactic mesh reinforcement during stoma reversal significantly decreases the incidence of stoma site incisional hernia without significant increase in the incidence of the stoma site wound infection.
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
For this study was approval from the institutional review board was obtained. IRB registration code: MD.19.01.136. Informed written consent: was taken from all cases before being enrolled in this work.
REFERENCES
1. Harries R, Torkington J. Stomal closure: strategies to prevent incisional hernia. Frontiers in surgery. 2018;5:28. eCollection 2018.
2. Memon Z, Qureshi S, Hakeem A. Outcome of closure of transient ileostomy at tertiary care hospital. In Med. Forum. 2019; 30(6): 123.
3. Cingi A, Cakir T, Sever A, Aktan A. Enterostomy site hernias: a clinical and computerized tomographic evaluation. Dis Colon Rectum. 2006;49(10):1559-63
4. Pine J, Stevenson, L. Intestinal stomas. Surgery (Oxford). 2017; 35(3):165-170.
5. Muysoms F, Miserez M, Berrevoet F, Campanelli G, Champault G, Chelala E, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13(4):407-414.
6. van Ramshorst G, Eker H, Hop W, Jeekel J, Lange J. Impact of incisional hernia on health-related quality of life and body image: a prospective cohort study. Am J Surg. 2012;204(2):144-50.
7. Kassem M, El-Haddad H. Polypropylene-based composite mesh versus standard polypropylene mesh in the reconstruction of complicated large abdominal wall hernias: a prospective randomized study. Hernia. 2016;20(5):691-700.
8. Sandy-Hodgetts K, Leslie G, Lewin G, Hendrie D, Carville K. Surgical wound dehiscence in an Australian community nursing service: time and cost to healing. J Wound Care. 2016;25(7):377-83.
9. Adell-Carceller R, Segarra-Soria M, Pellicer-Castell V, Marcote- Valdivieso E, Gamón-Giner R, Martin-Franco M, et al. Incisional hernia in colorectal cancer surgery. Associated risk-factors. Cir Esp. 2006;79(1):42-5.
10. Porrero J, Cano-Valderrama O, Castillo M, Marcos A, Tejerina G, Cendrero M, et al. Importance of mesh overlap on hernia recurrence after open umbilical hernia repair with bilayer prosthesis. Am J Surg. 2018;216(5):919-922.
11. Herbert G, Tausch T, Carter P. Prophylactic mesh to prevent incisional hernia: a note of caution. Am J Surg. 2009;197(5):595- 8; discussion 598
12. López-Cano M, Brandsma H, Bury K, Hansson B, Kyle-Leinhase I, Alamino J, et al. Prophylactic mesh to prevent parastomal hernia after end colostomy: a meta-analysis and trial sequential analysis. Hernia. 2017;21(2):177-189.
13. Krishnamurty, D, Blatnik, J, Mutch, M. Stoma complications. Clin Colon Rectal Surg. 2017;30(3):193-200.
14. Sier, M, Van Gelder, L, Ubbink, D, Bemelman, W, Oostenbroek, R. Factors affecting timing of closure and non-reversal of temporary ileostomies. Int J Colorectal Dis. 2015;30(9):1185-92.
15. Schreinemacher, M, Vijgen, G, Dagnelie, P, Bloemen, J, Huizinga, B, Bouvy, NIncisional hernias in temporary stoma wounds: a cohort study. Arch Surg. 2011;146(1):94-9.
16. Warren, J, Beffa, L, Carbonell, A, Cull, J, Sinopoli, B, Ewing, J, et al. Prophylactic placement of permanent synthetic mesh at the time of ostomy closure prevens formation of incisional hernias. Surgery. 2018;163(4):839-846.
17. Liu D, Banham E, Yellapu S. Prophylactic mesh reinforcement reduces stomal site incisional hernia after ileostomy closure. World J Surg. 2013;37(9):2039-45.
18. Pizza F, D’Antonio D, Arcopinto M, Dell’Isola C, Marvaso A. Safety and efficacy of prophylactic resorbable biosynthetic mesh in loopileostomy reversal: a case–control study. Updates Surg. 2020;72(1): 103-108
19. van Rooijen MM, Jairam AP, Tollens T, Jørgensen LN, de Vries Reilingh TS, Piessen G, et al. Outcomes of a new slowly resorbable biosynthetic mesh (Phasix®) in potentially contaminated incisional hernias: A prospective, multi-center, single-arm trial. Int J Surg. 2020;83:31-36.
20. Luijendijk R, Hop W, Van Den Tol M, De Lange D, Braaksma M, IJzermans J, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. 2000;343(6):392-8.
21. Maggiori L, Moszkowicz D, Zappa M, Mongin C, Panis Y. Bioprosthetic mesh reinforcement during temporary stoma closure decreases the rate of incisional hernia: a blinded, case-matched study in 94 patients with rectal cancer. Surgery. 2015;158(6):1651-7
22. Lambert D, Marceau S, Forse R. Intra-abdominal pressure in the morbidly obese. Obes Surg. 2005;15(9):1225-32.
23. Pierpont Y, Dinh T, Salas R, Johnson E, Wright T, Robson M, et al. Obesity and surgical wound healing: a current review. ISRN Obes. 2014;2014:638936. eCollection 2014.
24. Schreinemacher M, Vijgen G, Dagnelie P, Bloemen J, Huizinga B, Bouvy N. Incisional hernias in temporary stoma wounds: a cohort study. Arch Surg. 2011;146(1):94-9.
25. van Ramshorst G, Nieuwenhuizen J, Hop W, Arends P, Boom J, Jeekel J, et al. Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg. 2010;34(1):20-7.
26. Sharp S, Francis J, Valerian B, Canete J, Chismark A, Lee E. Incidence of ostomy site incisional hernias after stoma closure. Am Surg. 2015;81(12):1244-8.
27. Lorenz A, Kogler P, Kafka-Ritsch R, Öfner D, Perathoner A. Incisional hernia at the site of stoma reversal - incidence and risk-factors in a retrospective observational analysis. Int J Colorectal Dis. 2019; 34(7):1179-1187.
28. Riou J, Cohen J, Johnson Jr H. Factors influencing wound dehiscence. Am J Surg. 1992;163(3):324-30.
29. Walming S, Angenete E, Block M, Bock D, Gessler B, Haglind E. Retrospective review of risk factors for surgical wound dehiscence and incisional hernia. BMC Surg. 2017;17(1):19.
30. Gislason H, Søreide O, Viste A. Wound complications after major gastrointestinal operations. The surgeon as a risk factor. Dig Surg. 1999;16(6):512-4.
31. Niggebrugge AH, Trimbos JB, Hermans J, Steup WH, Van De Velde CJ. Influence of abdominal-wound closure technique on complications after surgery: a randomised study. Lancet. 1999;353(9164): 1563-7.
32. Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 2014;101(11):1439-47.
33. Yamamoto M, Tanaka K, Masubuchi S, Ishii M, Hamamoto H, Suzuki S, et al. Risk-factors for surgical site infection after stoma closure comparison between pursestring wound closure and conventional linear wound closure: propensity score matching analysis. Am J Surg. 2018;215(1):58-61.
Full Text Sources:
Abstract:
Views: 2715

Watch Video Articles
For Authors
Journal Subscriptions

Current Issue
Jun 2025
Supplements
Instructions for authors
Online submission
Contact
ISSN: 2559 - 723X (print)
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Open Access Statement
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Journal Metrics
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News