Surgery, Gastroenterology and Oncology

|
|
Background: laparoscopic colorectal surgery is considered the gold standard approach for management of surgical disease of the colon. De-functioning ileostomy is commonly used in cases of laparoscopic proctectomy to reduce the complications of anastomotic leak. There are different methods for specimen extraction from different abdominal wounds. One of them is to extract the specimen from ileostomy site.
Methodology: This was a prospective analytical study conducted on 30 patients that underwent laparoscopic proctectomy with specimen extraction from de-functioning ileostomy site at Ain Shams university hospitals during a period from June 2020 to December 2022 with follow-up period of 6 months after closure of ileostomy.
Results: Thirty patients were included, 2 patients (6.7%) developed stomal infection, one patient (3.3%) developed stoma stenosis. 3 patients (10%) had parastomal hernia (PSH) upon ileostomy closure, while 2 patients (6.7%) developed incisional hernia at ileostomy site at 6th month after closure of ileostomy.
Conclusion: Specimen extraction from diverting loop ileostomy site in cases of laparoscopic proctectomy is feasible and reproducible. It has the benefits of decreasing new incisions, good cosmetic outcomes, shortens duration of surgery, shortens hospital stay, with no significant increase in PSH or incisional hernia.
INTRODUCTION
Laparoscopic proctectomy is a minimally invasive surgical procedure that involves the removal of the rectum. It is commonly used to treat patients with rectal cancer in which resection of the rectum is followed by performing coloanal or low colorectal anastomosis (1). The lateral and distal margins of mesorectal excision have received the most attention as two crucial elements of optimum oncological resection. It has been shown that avoiding local recurrence of tumor in the pelvis requires precise dissection in the avascular plane surrounding the mesorectum to remove the mesorectum in its fascial envelope and to obtain a wide lateral margin (1).
Laparoscopic proctectomy may also be part of restorative proctocolectomy with ileal pouch anal anastomosis (IPAA) operation in which a permanent stoma is avoided. It is regarded as the best surgical option for people who have either familial adenomatous polyposis (FAP) or chronic ulcerative colitis (CUC), which is medically intractable or has dysplasia/malignancy (2).
Many studies have shown that compared to open surgery, minimally invasive colorectal surgery provides several benefits, including a quicker recovery of bowel function, less postoperative pain, and better cosmetic outcomes (3).
Specimen extraction after laparoscopic oncological surgery is one the point of interest aiming to preserve cosmesis outcome beside creation of a good view for tumor extraction without spillage or rupture. Pfannenstiel incision is the standard site for specimen extraction (4).
Temporary ileostomies are frequently performed on patients undergoing proctectomy to reduce the chance of anastomotic problems, including leakage and the need for additional surgery after rectal resection. Patients having temporary ileostomies are less likely to experience anastomotic leakage and peritonitis (4).
Presence of two open incisions (ileostomy and Pfannenstiel for specimen extraction) aroused the question if we can use one incision for both purposes. Enlarging the stoma aperture to extract the specimen and avoiding a second extraction incision is a typical method to reduce the number of incisions made when a stoma is necessary, better illustrating the idea of laparoscopic minimally invasive surgery, besides less operative time (6).
Nevertheless, there isn't enough information to say if removing a specimen through a stoma is more likely to cause morbidity, like stoma site hernia, stenosis, prolapse, or retraction (5). In this study we aimed to evaluate the feasibility and safety of specimen extraction via de-functioning ileostomy site in cases of laparoscopic proctectomy.
Patients and Methods
Study design
This is a prospective analytical study conducted at Ain Shams University hospitals over 30 patients who underwent laparoscopic proctectomy with specimen extraction from de-functioning ileostomy site during a period from June 2020 to December 2022 with follow-up period of 6 months after closure of ileostomy. We got informed written consent from all participants to share in this study. The ethical committee of the general surgery department approved the study.
Eligibility criteria for the study
We include all cases (males or females) aged from 18 to 70 years old who were candidate for laparoscopic proctectomy with covering loop ileostomy with radio-logical and pathological prove of resectable low rectal cancer, ulcerative colitis, and familial adenomatous polyposis. We excluded cases who were unfit for surgery, had previous major abdominal surgery, had metastatic or advanced rectal cancer or invading anal sphincters, patients who had anal incontinence, patients who were not planned to do diverting ileostomy, and patients with a psychiatric illness.
Preoperative preparation
All patients underwent preoperative clinical examination, routine preoperative investigations including carcinoembryonic antigen (CEA) for rectal cancer, serum albumin, hemoglobin. Preoperative pelvic magnetic resonance image (MRI) and positron emission with computerized tomography (PET-CT) were done for local and distant staging of rectal cancer. Colonoscopy was routinely performed in all cases. All locally advanced low rectal cancer patients received preoperative neoadjuvant chemoradiotherapy. The planned stoma site was marked by stoma nurse in three positions (standing, sitting, and supine).
Figure 1 - Port arrangement and a wound protector applied to planned ileostomy site

Operative technique
Prophylactic parenteral antibiotics (third generation cephalosporin and metronidazole) were given half hour before anesthesia induction. Laparoscopic approach was performed using 4 ports: 12 mm supraumbilical optical port for camera, 12 mm right iliac fossa port was inserted over the planned ileostomy site over the lateral border of the rectus abdominis muscle, 5 mm right hypochondrial port for the surgeon’s left hand and 5mm left lumbar assistant port (fig. 1).
Figure 2 - Specimen extraction from the planned ileostomy site, a wound protector applied
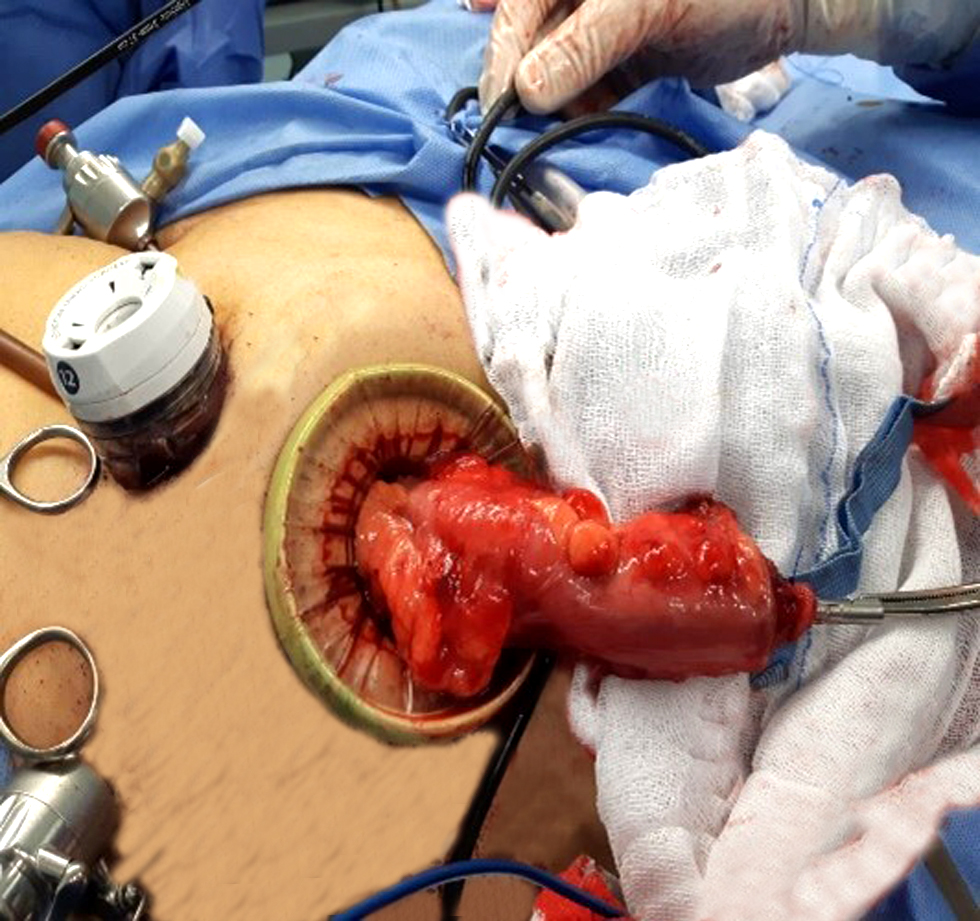
The technique of total mesorectal excision (TME) was followed in all cases including high ligation of inferior mesenteric artery (IMA) and medial to lateral colonic dissection. Ligation of inferior mesenteric vein (IMV) at the lower border of pancreas and splenic flexure mobilization were done in all cases to facilitate transverse colon mobilization and performing tension free anastomosis in the pelvis. Rectal dissection at the presacral holy plane was done. Transection of the distal margin was performed by Echelon flex 60™ stapler, blue cartridge (Ethicon). In cases of total proctocolectomy additional ports were added to the left hypochondrium and suprapubic region and medial to lateral approach was begun underneath ileocolic vessels to facilitate separation of the ascending colon from retroperitoneal structures. This was followed by clipping and division of ileocolic pedicle and middle colic vessels. This was followed by cutting the greater omentum and entering the lesser sac to separate transverse colon from stomach. The right lower quadrant port site was then extended, and Alexis® wound protector was then applied allowing delivery of the specimen (fig. 2) and transection of the proximal margin with no need to make a new incision.
Figure 3 - Anvil applied to the proximal colon following proctectomy

Anvil was then inserted to the proximal colon (fig. 3) or to J shaped small bowel pouch and secured by purse string proline 2-0 (fig. 4). Application of cap to Alexis port which allowed restoring the insufflation of the abdomen to continue the operative procedure without the need to close its site. This saves time and effort during the operation. Pneumoperitoneum was then reestablished and creation of tension free anastomosis via Echelon circular transanal stapler™ was done.
Figure 4 - Construction of ileal pouch after specimen extraction with applied wound protector

De-functioning loop ileostomy was then performed at the planned site for all patients (fig. 5).
Postoperative follow-up
Postoperative parenteral antibiotics (third generation cephalosporin and metronidazole) and analgesia were given to all cases. All patients were encouraged to commence oral diet once being open bowel (audible bowel sounds and passing flatus). Follow-up of the patients was carried out during hospital stay by evaluating postoperative pain, stoma site complications (infection, necrosis, stenosis, bleeding, retraction and prolapse) and other postoperative complications (anastomotic leakage, urinary retention, and bowel obstruction). Measurement of postoperative pain was done by using the “visual analog scale” (VAS) of 0 to 10, with 0 representing no pain and 10 representing the worst pain (6).
Figure 5 - Diverting loop ileostomy was created at the stoma site extraction

During routine outpatient clinic visits (after one week, two weeks and one month), clinical assessment of stoma complications and delayed leakage was performed for every patient. Follow up MRI was done at 1 month postoperative for all patients. Patients were referred to receive adjuvant treatment.
Routine distal loopogram was requested at 6th week after surgery. All patients who have clear operative bed with no anastomotic leakage were scheduled for closure of loop ileostomy in period from 8 to 12 weeks postoperatively. During ileostomy closure, the assessment of PSH was performed for every patient. Routine postoperative follow-up visits at 1 week, 2 weeks, 1 month, 3 months and 6 months to detect the incidence of wound infection and incisional hernia for every patient.
Follow-up
Clinical characteristics, operative outcomes, post-operative complications, and follow-up data were recorded in our database. Primary outcomes were assessment of postoperative pain, and stoma site complications (infection, necrosis, stenosis, bleeding, retraction and prolapse), and other postoperative complications (anastomotic leakage, urinary retention, and bowel obstruction). Secondary outcomes were the incidence of PSH during closure of ileostomy, and incidence of incisional hernia and wound infection at ileostomy site 6 months after closure.
Statistical analysis
Data management and statistical analysis were done using SPSS version 28 (IBM, Armonk, New York, United States). Statistical significance was assumed when the p value (two-sided) was less than 0.05. Categorical variables were reported as frequency (%), and quantitative variables were reported as mean ± standard deviation. Categorical variables were analyzed with Chi-square test. Quantitative variables were analyzed with a Wilcoxon rank-sum test.
Table 1 - Demographic characteristics of the patients who underwent laparoscopic proctectomy

RESULTS
Thirty patients were included in our study; 23 patients (76.6%) underwent low anterior resection for rectal cancer, while 7 patients (23.3%) underwent total proctocolectomy for FAP (4 patients) and UC (3 patients). 18 patients (60.0%) received neoadjuvant chemoradiotherapy. Other demographic characteristics of the patients are shown in
table 1.
The mean operative time of laparoscopic low anterior resection cases (n=23) was 224.43 min, the mean operative time of laparoscopic total proctocolectomy cases (n= 7) was 258.28 min, The overall mean operative time was 232.33± 17.24, min, while mean blood loss was 76.5±5.54. The mean hospital stay was 4.93 days ± 0.83 (table 2).
Table 2 - Operative and postoperative outcome data of patients who underwent laparoscopic proctectomy

Postoperative pain was put on VAS scale, the mean score was 3.13 at day 1 and dropped significantly to 1.2 at day 3. Regarding operative complications, 2 patients (6.7%) developed minor leakage from colorectal anastomosis. These cases were diagnosed clinically with persistent pelvic pain, confirmed radiologically by CT study, and were managed conservatively. There was no stoma prolapse nor stoma retraction in our study. Two patients (6.7%) developed peristomal infection (who were managed conservatively by antibiotics and stoma care by topical ointments). One patient (3.3%) developed stoma stenosis and was managed conservatively. We did not have any cases with urinary retention, bowel obstruction and other stoma complications (necrosis, bleeding, and retraction, and prolapse). Three patients (10%) had PSH upon ileostomy closure, while 2 patients (6.7%) developed incisional hernia at ileostomy site at 6th month after closure of ileostomy with no cases of wound infection (table 3). The cases of incisional hernia were planned to be repaired with mesh later.
Table 3 - Comparison between pain score at day 1 and at day 3 among all the studied patients

DISCUSSION
Early in the 1990s, laparoscopy for colorectal procedures was initially documented. Since then, there is no doubt about the advantages of laparoscopic colorectal surgery, which include earlier reduced post-operative pain, the restoration of bowel movement, and decreased rates of complications (7).
The primary surgical procedure currently used to treat middle and low rectal cancer is laparoscopic anterior resection, however anastomotic fistula is still a significant postoperative complication that must be avoided. Protective loop ileostomy is frequently carried out in laparoscopic low anterior rectal resection to decrease the prevalence of fistula and avoid its catastrophic effects (8).
Even though protective loop ileostomy is frequently employed in laparoscopic anterior resection of rectal cancer, we must be aware of its drawbacks. First, in cases of anastomotic leakage, local recurrence, and metastasis, the ileostomy runs the danger of becoming a permanent stoma. Second, the patients' quality of life is decreased since the leaking of feces would disturb them. Third, patients may have severe suffering because of ileostomy problems including stoma retraction, prolapse, necrosis, stricture, hemorrhage, skin irritation, and PSH. Therefore, it is crucial to have a better understanding of protective loop ileostomy indications and techniques (8).
Different authors from different centers all over the world have variable concepts for specimen extraction, some authors use Pfannenstiel incision, other authors tend to extend the umbilical incision, one of the proposed methods is using the planned stoma site as specimen extraction site. The patient won't have any incisions other than the port site, and the extraction site is turned into a stoma site that only requires routine stoma care and doesn't require any additional dressing, especially in cases with low rectal cancer. Marking of the right lower quadrant port before insufflation of the abdomen was performed for all the cases to be the optimum site of ileostomy (9).
Over 30 cases of laparoscopic proctectomy with specimen extraction via stoma site, our mean operative time was 232.33 min which is considered within the average when reviewing the literatures (263 min in Karakayali FY et al. study and 204.7 min in Lee K et al. study) (10,11).
In our study, the mean operative blood loss was 76.5 ml. Similarly, Wang P et al. found that the average estimated blood loss was 77.4 ml (12). In contrast to our study, the average blood loss of Li W et al. study was 100 ml, mostly because 76.3 % of their operated cases were inflammatory bowel disease more than ours (7).
In our study, the visual analog score of pain was 3.13 on day 1 and dropped to 1.2 on day 3. This was close to Karakayali et al. study, which showed that the median VAS score on postoperative days 1 and 3 were 4 and 2 respectively (10). In contrast, VAS score in Lee K et al. study was 5.1 at day 1 and 3.6 at day 3 mostly due to more postoperative stoma complication (22.7%) than our study (11).
Our mean hospital stay was 4.93 days. this was close to Li W. et al. study in which the mean length of hospital stay was 5 days (6). But it was slightly less than hospital stay in both Karakayali et al. study and, Lee K et al. (6 and 7.1 days respectively) (10,11). As regard non stoma postoperative complications in our study, the incidence of colorectal anastomotic leakage was 6.7% (managed conservatively) while we did not have other complications as urinary retention or bowel obstruction. With reviewing the literature, Li W.et al. study had no cases with anastomotic leakage while small bowel obstruction occurred in 2.9 % of their cases (7). The incidence of urinary retention and intestinal obstruction in Wang P et al. were very low (1.9 % and 0.6% respectively) (12). Lee K et al. had urinary retention in 7.1% of their cases (11).
Regarding stoma complications, we had 6.7 % of cases with peristomal infection (close to the incidence in Lee K et al. study which was 5.7%) (11). In contrast, the incidence of peristomal infection in Wang P et al. study was 2.6% (can be explained by more mean of BMI and diabetic cases in our study). In our study, the rate of stoma stenosis was 3.3%. which was slightly higher than Li W. et al. study in which, the stoma stenosis rate was 1.4% (7). In contrast, Wang P et al. study had no cases with stoma stenosis (12).
We had no cases with stoma prolapse or retraction. These complications were considered low in other studies. the incidence of prolapse in Wang P et al. and Li W et al. studies were 1.9%.and 1.4% respectively. While the incidence of stoma retraction in both studies were 0.6%, and 0.72 % respectively (7,12).
Regarding PSH, 3 patients (10%) developed it. These cases were incidentally discovered upon closure of ileostomy and were repaired without mesh. Our result matched with the findings in both Li W et al. and Lee K et al. studies (10.1 % and 11.3 % respectively) (7,11). In contrast, the incidence of PSH in Wang P et al. study was 2.6% mostly due to less incidence of stoma infection in their study (12). On the other side, Karakayali et al. study had 19 % of cases with PSH but they directly extending their ileostomy site then restitching to narrow it while we used Alexis to retract the port site rather than direct extension. Besides, their mean BMI was much less our result (24 % versus 31.93 %) (10). BMI was identified as a significant factor for PSH with multivariable analysis (11). The frequency of PSH after loop ileostomy reaches to 6.2% at a median of 3 months follow up and 9% at 4 months (14). The variation between studies in the incidence of PSH after loop ileostomy may depend on many factors as technique of stoma (aperture size and stoma location either through or lateral to rectus), stomal related complications and differences in follow-up until the ileostomy takedown procedure, besides, some authors had described parastomal prolapse as a subtype of PSH. The method of its diagnosis clinical or by CT may also falsely affect the true incidence (7).
Regarding stoma site incisional hernia in our study, 2 patients (6.7%) developed incisional hernia at ileostomy site at 6th month after closure of ileostomy. In contrast, the incidence of stoma site hernia in Li W et al. study, was 2.7% secondary to less incidence of PSH in their study (7). But Karakayali et al. study had slightly higher incidence of stoma site hernia (10%) mostly secondary to higher incidence of PSH in their study (10). The increased risk of stoma site hernia is referred to constant tension on the fascia from Alexis port and traction from the instruments (13).
Although stoma complications may be a result of specimen extraction via stoma site, but this point is of no clinical significance due to early takedown of the stoma, but to be considered in permanent stoma (7). While the stoma site hernia is considered the point of interest in this issue which is considered within accepted incidence with avoiding an extra incision for specimen extraction rather than stoma site (7). In our study, we thought that using Alexis protector is a beneficial guard against contamination or malignant implantation with specimen extraction.
The current study has some limitations as small sample size, a comparative study with conventional method is needed to emphasize the results, a longer follow up duration is also needed to evaluate the long-term outcomes.
CONCLUSION
Specimen extraction from diverting loop ileostomy site in cases of laparoscopic proctectomy is feasible and reproducible. It has good cosmetic outcomes with less operative time, less hospital stay, with no significant increase in PSH or incisional hernia.
Conflict of interest
The authors declare that they have no conflict ofinterest.
Funding and financial support
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
REFERENCES
- Read TE, Marcello PW. Laparoscopy for rectal cancer: the need for randomized trials. Clin Colon Rectal Surg. 2006;19(1):13-8.
- Opoku D, Hart A, Thompson DT, Tran CG, Suraju MO, Chang J, et al. Equivalency of short-term perioperative outcomes after open, laparoscopic, and robotic ileal pouch anal anastomosis. Does procedure complexity override operative approach? Surg Open Sci. 2022;9:86-90.
- Morelli L, Guadagni S, Mariniello MD, Furbetta N, Pisano R, D’Isidoro C, et al. Hand-assisted hybrid laparoscopic–robotic total proctocolectomy with ileal pouch-anal anastomosis. Langenbecks Arch Surg. 2015;400(6):741-8.
- Peng D, Yu DL, Liu XY, Tao W, Kang B, Zhang H, et al. Does temporary ileostomy via specimen extraction site affect the short outcomes and complications after laparoscopic low anterior resection in rectal cancer patients? A propensity score matching analysis. BMC Surg. 2022;22(1):263.
- Wu A, Wu B, Shu X, Cao Y, Zeng Q, Li Z, et al. Application of a Temporary Ileostomy via Median Specimen Extraction Site in Laparoscopic Low Anterior Resection. Research Square; 2021.
- Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15 Suppl 1(Suppl 1):S17-24.
- Li W, Benlice C, Stocchi L, Kessler H, Gorgun E, Costedio M. Does stoma site specimen extraction increase postoperative ileostomy complication rates? Surg Endosc. 2017;31(9):3552-3558.
- Liu C, Zhang J, Li L, Zhang L, Shang L, Ma Y. Comparison of specimen extraction site and another site for protective loop ileostomy in laparoscopic low anterior rectal resection: a retrospective comparative study. Langenbecks Arch Surg. 2023;408(1):151.
- DeSouza A, Domajnko B, Park J, Marecik S, Prasad L, Abcarian H. Incisional hernia, midline versus low transverse incision: what is the ideal incision for specimen extraction and hand-assisted laparoscopy? Surg Endosc. 2011;25(4):1031-6.
- Karakayali FY, Tezcaner T, Moray G. Specimen extraction from the defunctioning ileostomy site or pfannenstiel incision during total laparoscopic low anterior resection for rectal cancer. J Laparoendosc Adv Surg Tech A. 2015;25(5):380-5.
- Lee KY, Park JW, Lee KY, Cho S, Kwon YH, Kim MJ, et al. Safety of temporary ileostomy via specimen extraction site in rectal cancer patients who underwent laparoscopic low anterior resection. Sci Rep. 2019;9(1):2316.
- Wang P, Liang JW, Zhou HT, Wang Z, Zhou ZX. Surgical specimen extraction via a prophylactic ileostomy procedure: a minimally invasive technique for laparoscopic rectal cancer surgery. World J Gastroenterol. 2018;24(1):104-111.
- Nastro P, Knowles CH, McGrath A, Heyman B, Porrett TR, Lunniss PJ. Complications of intestinal stomas. Br J Surg. 2010;97(12): 1885-9.
- Caricato M, Ausania F, Ripetti V, Bartolozzi F, Campoli G, Coppola R. Retrospective analysis of long-term defunctioning stoma complications after colorectal surgery. Colorectal Dis. 2007; 9(6):559-61.
- Antoniou SA, Morales-Conde S, Antoniou GA, Granderath FA, Berrevoet F, Muysoms FE, et al. Single-incision laparoscopic surgery through the umbilicus is associated with a higher incidence of trocar-site hernia than conventional laparoscopy: a meta-analysis of randomized controlled trials. Hernia. 2016;20(1):1-10.
Full Text Sources:
Abstract:
Views: 1559

For Authors
Journal Subscriptions

Sept 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News