Surgery, Gastroenterology and Oncology

|
|
Background: The fast-track program of laparoscopic cholecystectomy has proven its efficacy in elective surgery and could hypothetically improve outcomes in acute settings.
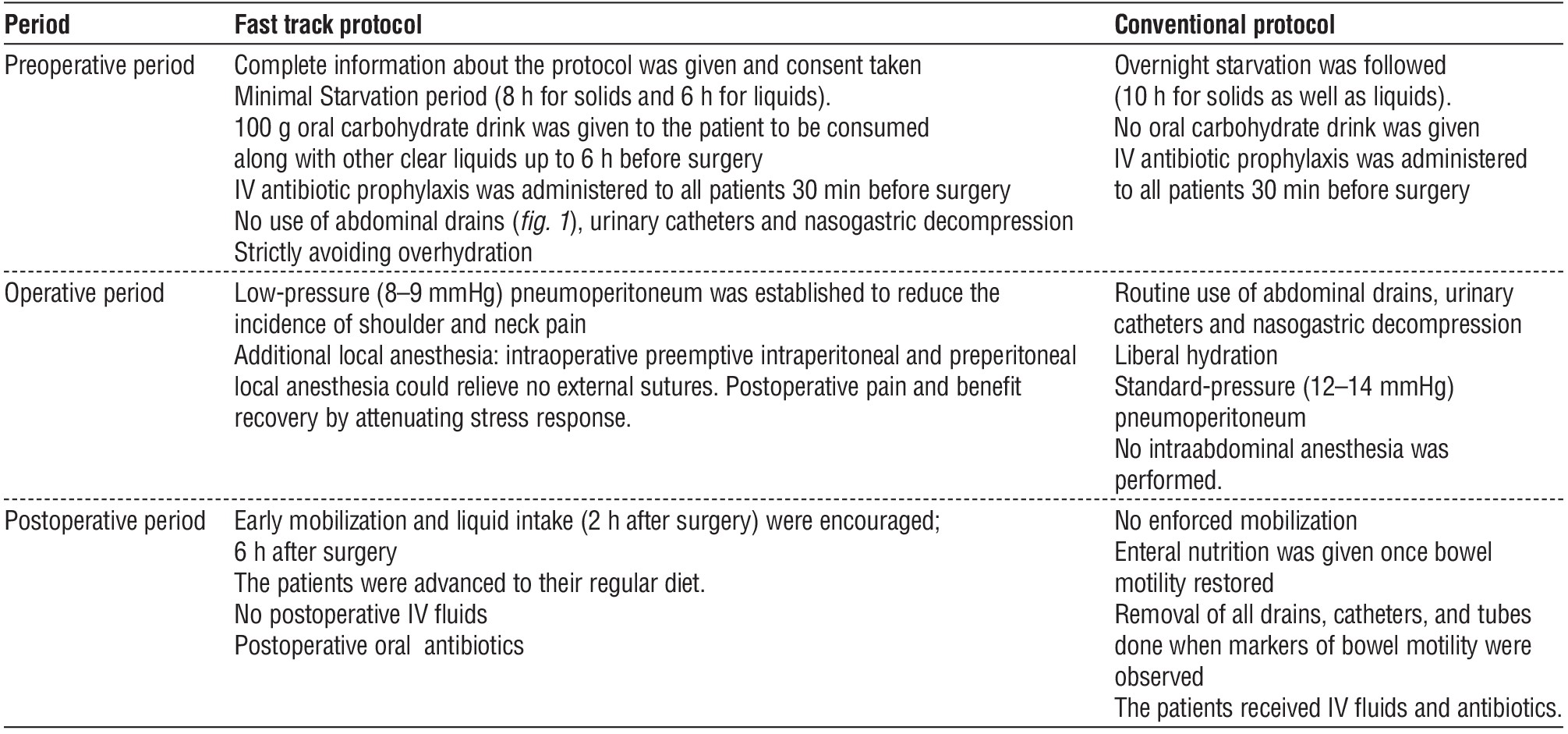
Materials and Methods: The fast-track protocol included minimizing drain use; local anesthesia; low-pressure pneumoperitoneum; early mobilization and oral diet. The primary outcome was postoperative pain, length of stay (pLOS), and the total cost. ZnO-Agar nanocomposite was synthesized by a microwave method.
Results: Modified protocol reduced median pLOS to 0.9 days vs 1.6 days in the controls (p<0.001). Ninety-five (86%) of fast-track patients were discharged within 6h (p<0.001) after surgery; 0 readmissions were reported. Postoperative pain intensity assessed on the visual analog scale was significantly lower in the fast-track group (p<0.0001). The severity of shoulder and neck pain was lower but its incidence was similar. Peristalsis recovery was achieved earlier in the study group. Patient satisfaction and total cost were better in the study group. ZnO-Agar nanocomposite (ZOA NC) possesses antimicrobial activity and enhances wound healing.
Conclusion: The fast-track program for laparoscopic cholecystectomy has advantages over the traditional approach.
Introduction
Over the past ten years, fast-track strategies have gained increasing traction and contributed to the advancement of postoperative treatment strategies (1). Research has shown that a multidisciplinary approach to surgical patient care that emphasizes early nutrition and ambulation can hasten recovery, help with early hospital discharge, limit the use of opioid painkillers, and vigorously prevent postoperative nausea and vomiting (PONV) while maintaining patient safety (2).
Multimodal therapy paths aimed at preserving preoperative organ function and lowering the intensity of the stress reaction during surgery in order to promote rapid recovery following surgery (3). Fast-track protocols' essential components include preoperative counselling, food optimization, comprehensive analgesic and anesthetic regimens, and early mobilization. Despite the overwhelming evidence that Fast-track protocol operations improve outcomes, they go against accepted surgical practice and are therefore difficult to implement (4).
In the 1980s, the approach to laparoscopic cholecystectomy was initially used, decisively replacing the open technique in the accepted method. The laparoscopic approach requires fewer incisions and causes less pain after surgery. Numerous studies comparing the same-day discharge (SDD) against the overnight hospital stay (OHS) after LC have found no differences in death, adverse events, or readmission rates (5).
The history of the use of zinc as a biologically active mineral goes back to ancient times. Zinc ointment was used for skin diseases and to accelerate wound healing in ancient Egypt 5000 years ago (6). Zinc is an important element for the functioning of a wide range of physiological functions of living organisms (7). Zinc participates in carbohydrate metabolism through a zinc-containing hormone–insulin, and is also necessary for the absorption of vitamin A. Zinc also has anti-inflammatory properties (8-10).
Materials and methods
Fabrication of ZnO-Agar nanocomposite (ZOA NC)
ZnO–Agar nanocomposite was synthesized by a microwave method according to Blinov et al. About 1.0 g of the purified Agar was dissolved in 100 ml of distilled water at 95ºC under magnetic stirring. After complete dissolution, 100 ml of 0.1 M ZnCl2 solution was added in to the Agar solution drop wise. 0.1 M NaOH was
prepared and added with stirring to zinc chloride agar mixture solution to the set pH of 10. The mixture was kept in a domestic microwave oven at 170 W for 25 minutes. The reaction was carried at 3 minutes interval. After the reaction a milky white composite was obtained which indicates the formation of ZnO nanoparticles. The composite was washed with distilled water repeatedly in order to remove the excess agar. The obtained sample was dried at 80ºC in an Oven (11).
Characterization of ZOA nanocomposite
Fourier transform infrared (FT-IR) analysis was performed using a Perkin Elmer spectrophotometer.
X-ray powder diffraction (XRD) datas were collected using an X -ray diffractometer (Bruker, AXS) with Cu-Kα radiation (0.15406 nm). The surface morphologies of the particles were observed by a field-emission scanning electron microscope (SEM) (JEOL, JSM - 6700F).
Clinical surgical
This study was a prospective randomized controlled trial including 220 patients candidate for laparoscopic cholecystectomy due to diseased gallbladder, the
indication of cholecystectomy was based on review of clinical and imaging reports were identified. Those patients were subjected to laparoscopic cholecystectomy at Theodor Bilhariz Research Institute Hospital between 2021 and 2023. Patients were randomized into two groups (Group A: Patients received FT perioperative care & Group B: Patients received traditional perioperative care) each group consisit of 110 patients (table 1).
A sealed opaque envelope (according to the computer generated random sequence) will be used to determine the appropriate program of care. All laparos-copic surgeries will be performed by experienced biliary surgeons.
Inclusion criteria included
• Age 18-75 years old.
• Diagnosis of acute cholecystitis defined by the presence of at least 2 of the following:
• Abdominal pain in upper right quadrant,
• Murphy's sign.
• Leukocytosis >10 × 103/μl.
• Oral temperature < 36.5°C or > 38°C.
• Cholelithiasis (stones/sludge).
• Ultrasound signs of cholecystitis.
• Expected to require at least an overnight hospital admission after surgery; and
• Provide written informed consent to participate in FAST.
Exclusion criteria included
• Patients requiring emergent surgery or emergent interventions for another reason.
• Patients whose therapeutic anticoagulation is not reversible.
• Patients with a history of heparin-induced
thrombocytopenia and current use of warfarin with an INR ≥1.5.
• Pregnant patients.
Investigation of healing ability of ZnO-Agar nanocomposite
An experiment was carried out on patients to study the effect of an Agar nanocomposite based on ZnO NPs for the healing process of wounds, where the composite was added for the duration of the experiment ten days.
Results
Characterization of ZnO-Agar
nanocomposite gel
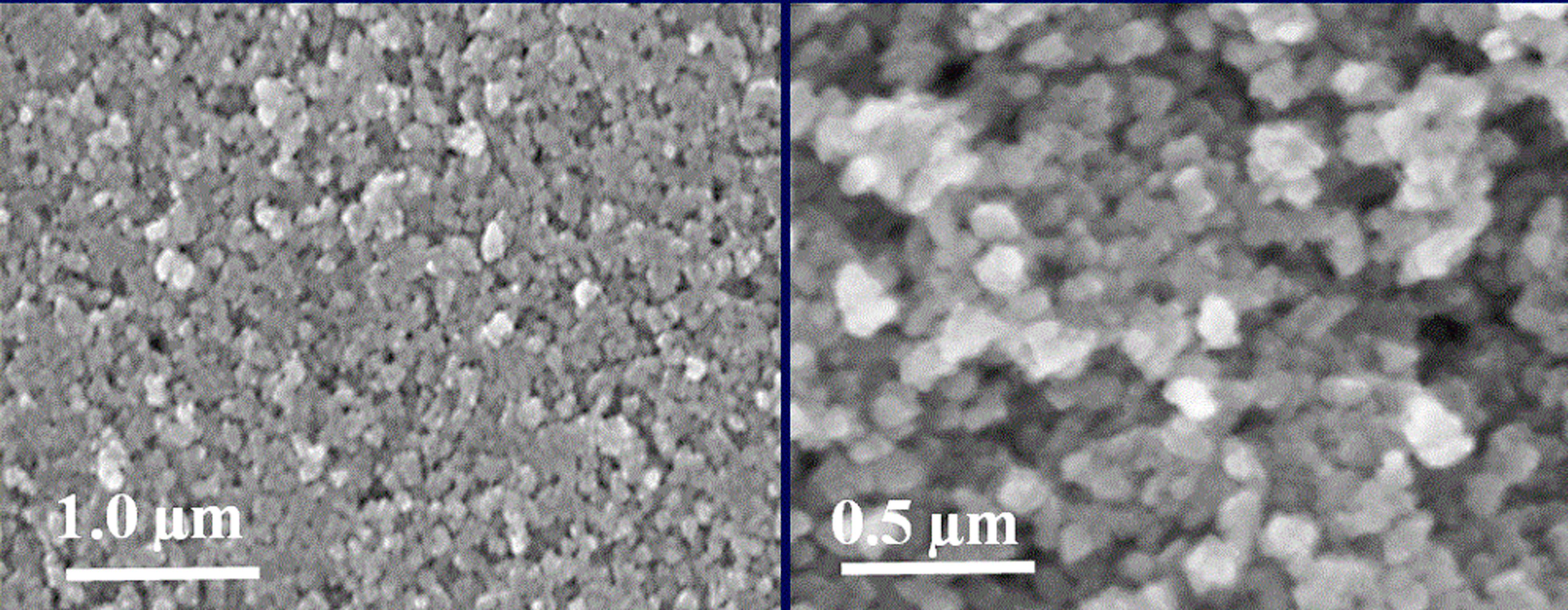
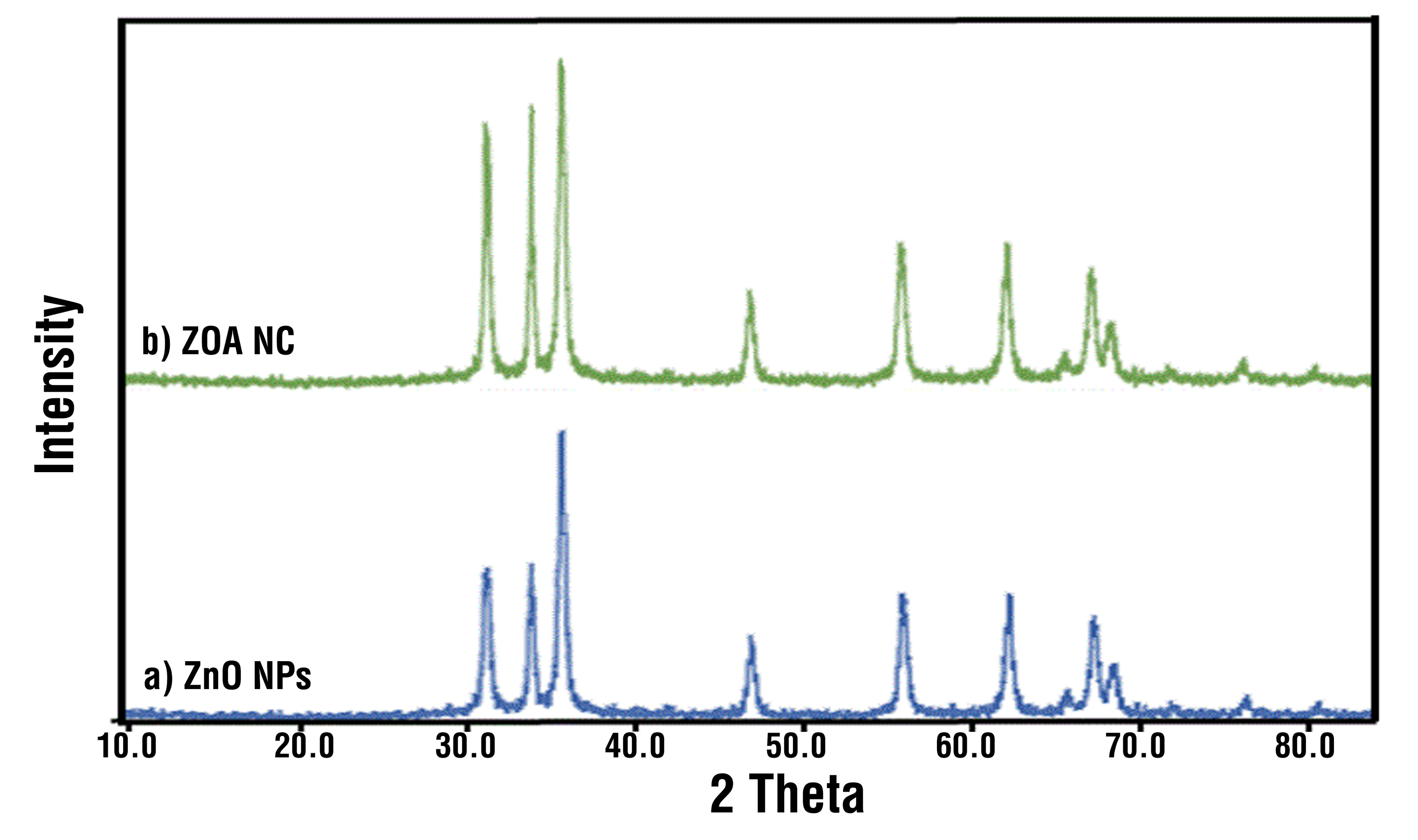
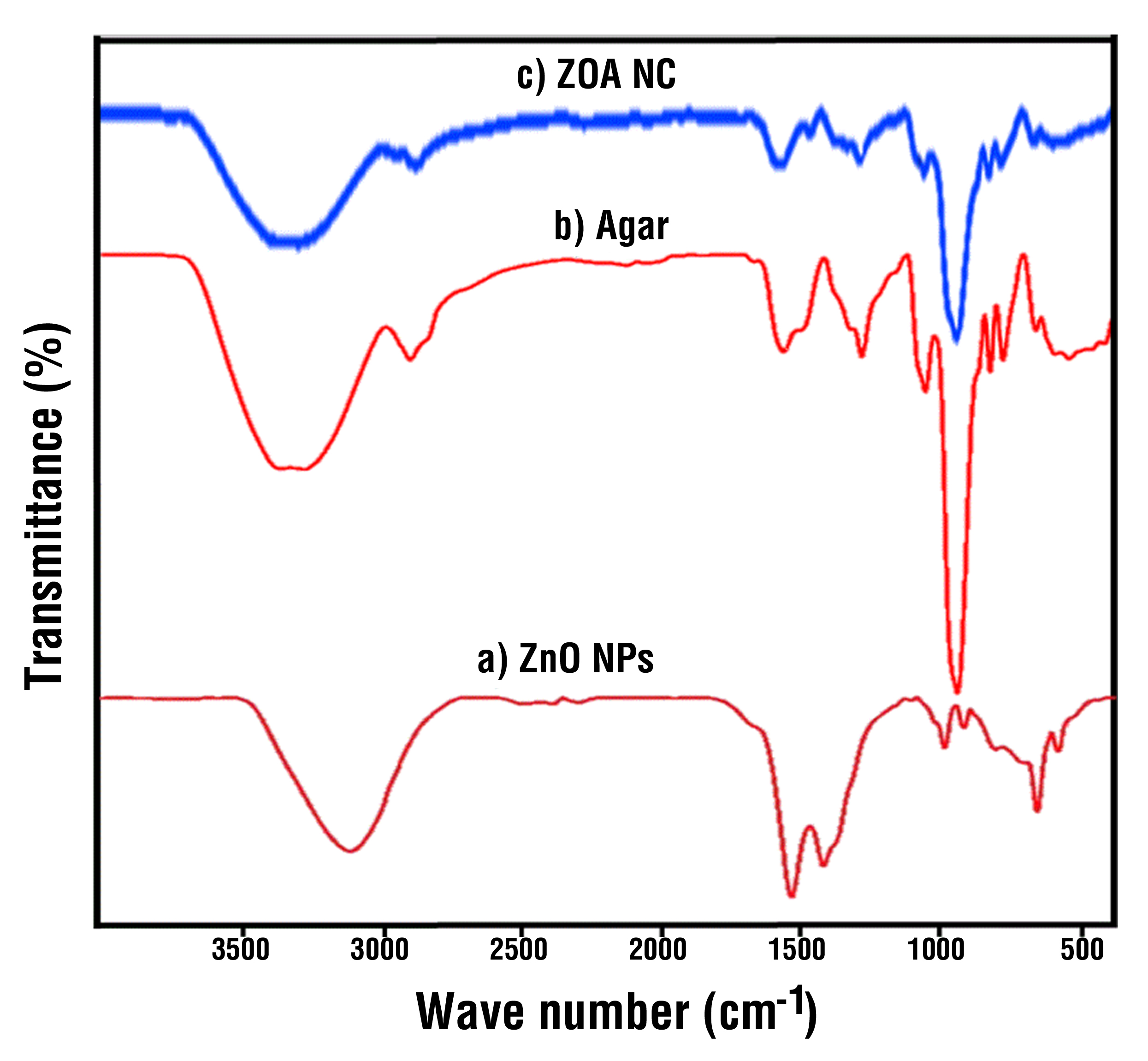
The micrograph of nanoscale ZnO-Agar NC was studied by SEM as shown in fig. 1. The SEM images showed that nanocomposite consists of irregularly lamellar-shaped aggregates with average size 165 nm. Fig. 2 shows the XRD pattern of the ZnO-Agar NC. There are mainly three characteristic peaks between 30 and 40 degrees for the pure ZnO NPs due to the high degree of crystallinity. These peaks are still represented in the spectrum of the ZnO-Agar NC, which indicates the stability crystallization of the nanocomposite. As a result of the analysis of IR spectra fig. 3, it was found that in the spectra of ZnO-Agar NC in the range from 1350 to 1450 cm−1, there is a significant drop in the intensity of the bands characterizing the deformation vibrations of theionized charged group–OH. Thus, it was established that the interaction of ZnO NPs occurs through the charged hydroxyl group of agar (11).
Clinical study
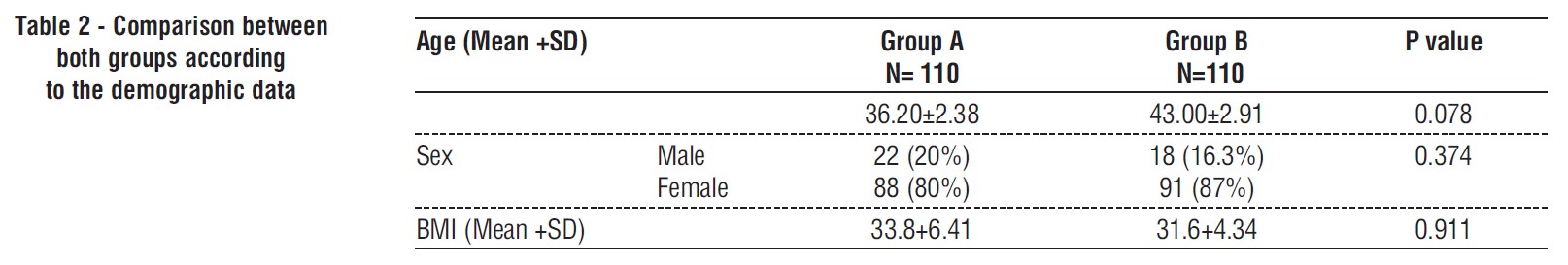
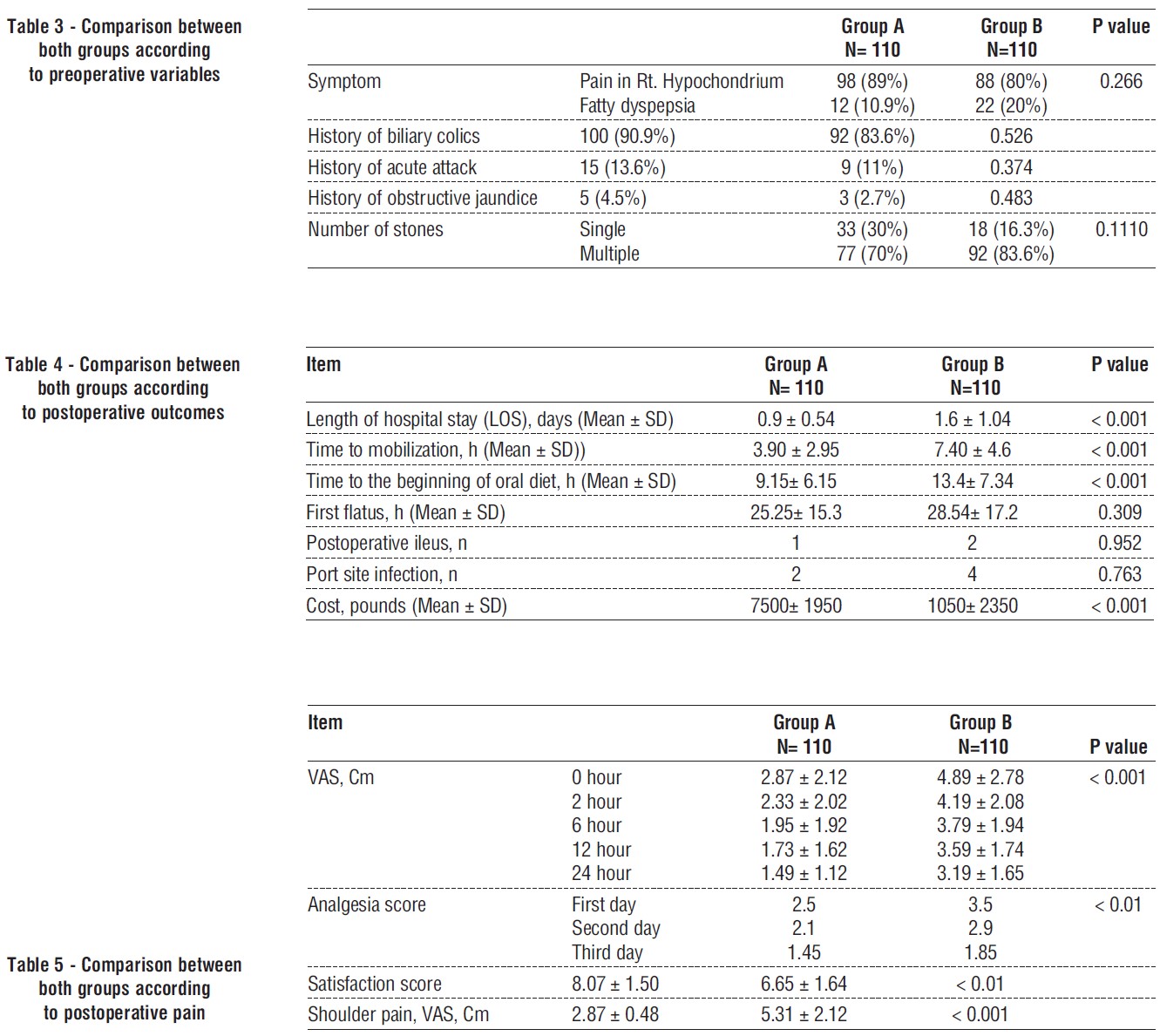
During the study period, November 4, 2021 through April 5, 2023, 220 laparoscopic cholecystectomies were performed in Theodor Bilhariz Research Institute Hospital. Fast-track perioperative care group (Group A) was compared with traditional perioperative care group (Group B) (tables 2-5).
Discussion
Day surgical management for elective LC became popular in the 1990s and was taken into account for outpatient postoperative recovery (12). According to Calland et al., same-day discharges increased from 21 to 72% after establishing a clinical pathway for laparos-copic cholecystectomy, and the overall cost of
treatment decreased by 17.5% without affecting patient satisfaction or safety (13).
Additionally, Cash et al. found that an LC outpatient regimen enhanced the rate of outpatient management with no increase in morbidity or mortality (14). Greater same-day discharge rates with low complication rates and high patient satisfaction can be achieved by cost-effective practices, increased patient education, and initiatives to remove common postoperative difficulties (such as nausea and discomfort) (13,15,16).
The predicted admission and readmission rates for an outpatient LC are 10% and 5%, respectively (17), with the majority of patients successfully released within 6 to 8 hours of postoperative surveillance (18,19). The acute care setting is always looking for ways to cut down on LOS while still providing excellent care and a high level of patient satisfaction. Nursing care is the main focus of a fast-track protocol. Using protocol milestones, nurses may manage the postoperative experience at a steady pace. According to earlier research, a fast-track program reduces the quantity of nursing care needed for each patient (20). Additionally, informed patients heal more quickly, experience less pain after surgery, and experience less anxiety (21).
In light of this, the ''Fast-Track'' protocol's foundation starts with the initial patient consultation, continues in the operating room, and is dependent on pain management and nursing care during postoperative recovery. Our research shows that a fast-track approach for large volume, fairly predictable surgical operations can save hospital costs without sacrificing patient care. As anticipated, there was little difference in the demographics, satisfaction, complication, and readmission rates of patients who underwent urgent laparoscopic cholecystectomies between the historical (PRE) and post implementation cohorts (POST), and there was a tendency towards shorter lengths of stay (LOS) between the protocol-compliant cohorts and the historical cohorts. It would seem that the implementation of a protocol resulted in a shift in attitude towards earlier discharge, regardless of whether patients were actually put on the program.
When patients were able to follow the procedure, the LOS was cut by one day without a rise in complications, readmissions, or a drop in patient satisfaction ratings. Reduced inpatient stays are expected to result in cost and staffing savings. There was a sizable decrease in both LOS and hospital costs when comparing those in the FT cohort with those in the NFT cohort. Over one day of LOS was drastically cut, and hospital bills were on average lowered by 3500 pounds. Patients thus did not even need to finish the FT procedure in order to save money. Whether or whether patients were actually put on the procedure, it would seem that the introduction of the program caused a shift in thinking towards early discharge.
Even though 3500 pounds may seem like a modest amount, when multiplied by the anticipated number of cholecystectomy patients who are admitted each year, the savings to the healthcare system might total millions.
The postoperative experience was standardized by this regimen, which also addressed the problems like pain and nausea that regularly caused our patient population's LOS to increase. Implementing multimodal analgesia in the operating room, post-anesthesia care unit, or as soon as the patient is admitted to the in patient care floor following surgery is where the pathway starts. For the prevention and treatment of postoperative laparoscopic discomfort, multimodal analgesia is advised (22). Postoperative pain can be effectively managed by using incisional local anaesthetics, NSAIDs, dexamethasone, elimination of residual carbon dioxide, and postoperative opioids (23).
The literature review reveals that these modalities lessen discomfort and enable earlier discharge, allowing for the management of more patients as outpatients (24,25). All patients participating in the fast-track procedure received acetaminophen and ibuprofen /ketorolac unless contraindicated. On being transferred out of the post-anesthesia care unit, oral painkillers were started. The factors affecting preoperative LOS were not addressed, although this may call for future research. To prevent overeating after surgery and to lessen postoperative nausea and vomiting, the diet was limited to simply liquids with toast or crackers. With a 30% frequency, postoperative nausea and vomiting are the most frequent side effects that patients experience after surgery under general anaesthesia (26). However, after LC, the incidence of postoperative nausea and vomiting is higher, ranging from 46 to 75% (27,28). These symptoms may be a result of general anaesthetics and opioids delaying the gastric emptying process.
Six hours following the end of the procedure was the target completion time for the rapid tract protocol. Four hours on the inpatient unit were allotted in the timeline and milestone documentation. As a result, nursing care was provided much more quickly than usual. The nurses had to change their focus due to the policy. Our study demonstrates that laparoscopic cholecystectomy patients can be successfully handled using an FT procedure and obtains noticeably shorter LOS, comparable results, high patient satisfaction with their care, and decreased hospital expenses. A fast-track protocol's success appears to be directly related to multimodal pain treatment. Other patients and procedures handled by the ACS service that potentially profit from a fast-track protocol should be identified and evaluated in further research.
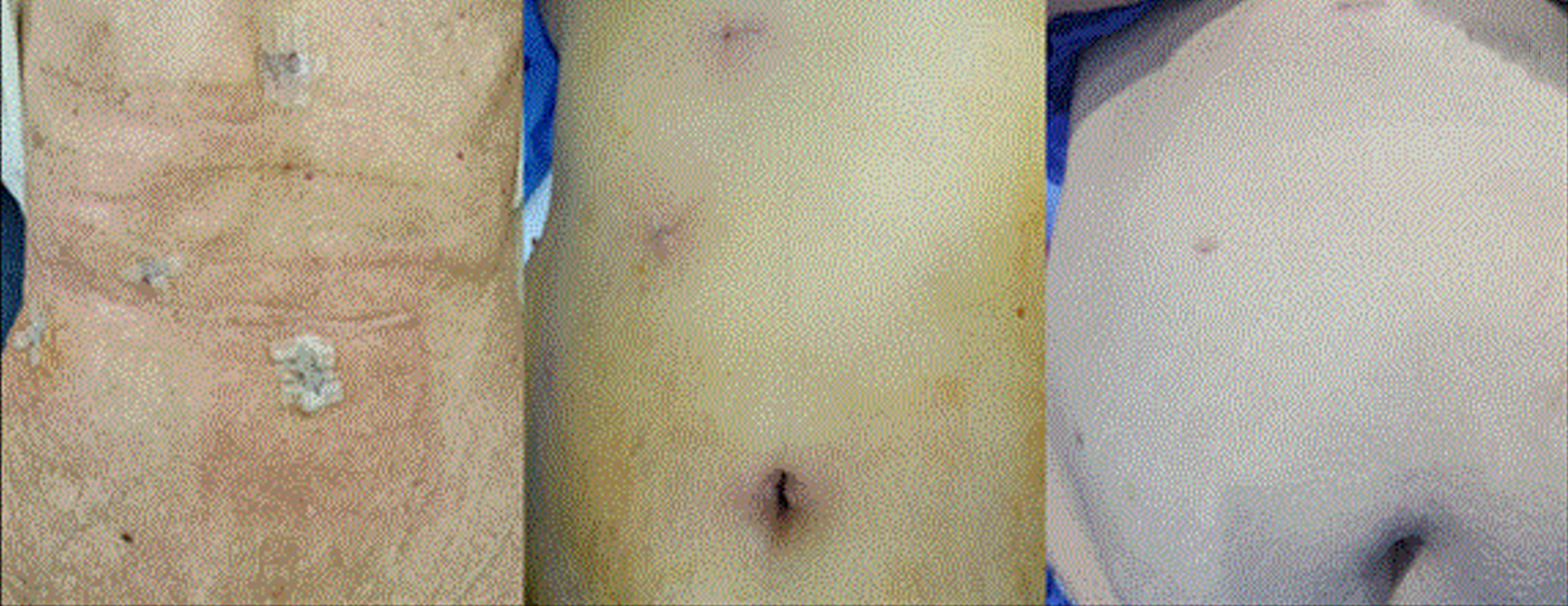
The using of Zn-Agar nanocomposite was helping for accelerating healing, where the wounds healed after ranging from 5 to 8 days only, where they have antimicrobial activity and anti-inflammatory effects that allow for fast healing of wounds (fig. 4) (8 -11).
Conclusion
In addition to optimizing patient functional rehabilitation and quality of life, the fast-track route for electives experiencing laparoscopic cholesteatoma is healthy. As a result, mean postoperative hospitalization and complete hospital stay with lower complications and little chance of rehabilitation have declined significantly. The average rate of healing of wounds is higher than the control group. An experimental study of a gel of ZnO NPs modified with agar has shown the effectiveness of its use in the healing of skin wounds.
Acknowledgment
This work was supported by the General Surgery Department, Anaesthesiology Department, Nano-Environmental Unit (NEU) Theodor Bilharz Research Institute (TBRI), Egypt, and Dr. Alia Maghney, Undergraduate student at the Faculty of Medicine, Cairo University, for its participation in data collection, analysis, and helping for manuscript writing.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval and consent to participate
The study was approved by the Research Ethics Committee at Theodor Bilharz Research Institute, Egypt (Approval Number: PT-707), and informed consent was obtained from the patients through the institutional consent form, which included permission to use their data for research purposes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
1. Papandria D, Sebastião YV, Deans KJ, Diefenbach KA, Minneci PC. Examining length of stay after commonly performed surgical procedures in ACS NSQIP pediatric. J Surg Res. 2018;231:186-194.
2. Schumann R, Ziemann-Gimmel P, Sultana A, Eldawlatly AA, Kothari SN, Shah S, et al. Postoperative nausea and vomiting in bariatric surgery: a position statement endorsed by the ASMBS and the ISPCOP. Surg Obes Relat Dis. 2021;17(11):1829-1833.
3. Aguilar-Nascimento JE, Bicudo Salomão A, Caporossi C, Diniz BN. Clinical benefits after the implementation of a multimodal peri-operative protocol in elderly patients. Arq Gastroenterol. 2010; 47(2):178-83.
4. Ahmed J, Khan S, Lim M, Chandrasekaran TV, MacFie J. Enhanced recovery after surgery protocols–compliance and variations in practice during routine colorectal surgery. Colorectal Dis. 2012; 14(9):1045-51.
5. Sartelli M, Chichom-Mefire A, Labricciosa FM, Hardcastle T, Abu-Zidan FM, Adesunkanmi AK, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017;12:29.
6. Feijó GDS, Jantsch J, Luz Correia L, Eller S, Vieira Furtado-Filho O, Giovenardi M, et al. Neuroinflammatory responses following zinc or branched-chain amino acids supplementation in obese rats. Metab Brain Dis. 2022;37(6):1875-1886.
7. Ibrahim NK, Almajeed MA, Kadhum HJ. Essential Role of Zinc in Human Immunity: A Subject Review. Educ Med J:1-9.
8. Park H, Kim W, Kim D, Jeong S, Jung Y. Mesalazine activates adenosine monophosphate-activated protein kinase: implication in the anti-inflammatory activity of this anti-colitic drug. Curr Mol Pharmacol. 2019;12(4):272-280.
9. Read SA, Obeid S, Ahlenstiel C, Ahlenstiel G. The role of zinc in antiviral immunity. Adv Nutr. 2019;10(4):696-710.
10. Kanwar A, Sharma AA. A review on role of zinc as a potent immunity boosting agent. Materials Today Proceedings. 2022;68(5–6):880-885.
11. Blinov D, Maharana S, Bouzelou F, Casadio C, Gjerløw E, Jormanainen J, et al. The RoboPol sample of optical polarimetric standards. A&A. 2023;677:A144.
12. Jaschinski T, Mosch CG, Eikermann M, Neugebauer EA, Sauerland S. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;11(11):CD001546.
13. Calland JF, Tanaka K, Foley E, Bovbjerg VE, Markey DW, Blome S, et al. Outpatient laparoscopic cholecystectomy: patient outcomes after implementation of a clinical pathway. Ann Surg. 2001;233(5):704-15.
14. Cash CL, Frazee RC, Abernathy SW, Childs EW, Davis ML, Hendricks JC, Smith RW et al. A prospective treatment protocol for outpatient laparoscopic appendectomy for acute appendicitis. J Am Coll Surg. 2012;215(1):101-5; discussion 105-6.
15. Dyas AR, Henderson WG, Madsen HJ, Bronsert MR, Colborn KL, Lambert-Kerzner A, et al. Development and validation of a prediction model for conversion of outpatient to inpatient surgery. Surgery. 2022;172(1):249-256.
16. Ahmad NZ, Byrnes G, Naqvi SA. A meta-analysis of ambulatory versus inpatient laparoscopic cholecystectomy. Surg Endosc. 2008; 22(9):1928-34.
17. Lawrence KNABM, Boller AM, Mahvi DM. Cholecystitis. Surg Clin North Am. 2014;94(2):455-70.
18. Carlomagno N, Tammaro V, Scotti A, Candida M, Calogero A, Santangelo ML. Is day-surgery laparoscopic cholecystectomy contraindicated in the elderly? Results from a retrospective study and literature review. Int J Surg. 2016;33 Suppl 1:S103-7.
19. Vaughan J, Selvan Gurusamy K, Davidson BR. Day-surgery versus overnight stay surgery for laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2013;(7):CD006798.
20. Hübner M, Addor V, Slieker J, Griesser AC, Lécureux E, Blanc C, et al. The impact of an enhanced recovery pathway on nursing workload: A retrospective cohort study. Int J Surg. 2015;24(Pt A):45-50.
21. Brodersen F, Wagner J, Güntac Uzunoglu F, Petersen-Ewert C. Impact of preoperative patient education on postoperative recovery in abdominal surgery: a systematic review. World J Surg. 2023; 47(4):937-947.
22. Baird DLH, Simillis C, Kontovounisios C, Rasheed S, Tekkis PP. Acute appendicitis. BMJ. 2017;357:j1703.
23. Barazanchi AWH, MacFater WS, Rahiri J-L, Tutone S, Hill AG, Joshi GP. Evidence-based management of pain after laparoscopic cholecystectomy: a prospect review update. Br J Anaesth. 2018;121(4): 787-803.
24. Fregoso G, Wang A, Tseng K, Wang J. Transition from acute to chronic pain: evaluating risk for chronic postsurgical pain. Pain Physician. 2019;22(5):479-488.
25. Peng K, Ji F-h, Liu H-y, Wu S-r. Ultrasound-guided transversus abdominis plane block for analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis. Med Princ Pract. 2016; 25(3):237-46.
26. Sridharan K, Sivaramakrishnan G. Drugs for preventing post-operative nausea and vomiting in patients undergoing laparoscopic cholecystectomy: Network meta-analysis of randomized clinical trials and trial sequential analysis. Int J Surg. 2019;69:1-12.
27. Gauchan S, Thapa C, Shakya P, Bhattarai R, Shakya S. Ondansetron and Granisetron for prevention of postoperative nausea and vomiting following laparoscopic cholecystectomy. JNMA J Nepal Med Assoc. 2014;52(193):682-6.
28. Weibel S, Rücker G, Eberhart LHj, Pace NL, Hartl HM, Jordan OL, et al. Drugs for preventing postoperative nausea and vomiting in adults after general anaesthesia: a network meta-analysis. Cochrane Database Syst Rev. 2020;10(10):CD012859.
Full Text Sources:
Abstract:
Views: 2482

For Authors
Journal Subscriptions

Jun 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News