Surgery, Gastroenterology and Oncology

|
|
Introduction: Volvulus of the ascending colon is a rare cause of large bowel obstruction and presents because of its mesentery with excessive mobility allowing it to rotate on its axis. It is usually due to a congenital or acquired anatomical variation. Objective: To describe volvulus of the ascending colon as a rare complication in a young patient, whose diagnosis was mistaken for sigmoid volvulus and diaphragmatic hernia.
Case report: We present the case of a 27-year-old woman who presented with periumbilical abdominal pain, nausea, vomiting and absence of bowel movements which, according to imaging tests, suggested a sigmoid volvulus and a diaphragmatic hernia at the beginning. After performing a laparotomy, a volvulus of the ascending colon was found up to the middle third of the transverse colon rotated 180º clockwise, a right hemicolectomy was performed plus resection of 10 cm of the distal ileum; it was decided to close the distal colonic end in two planes and perform an ileostomy.
Conclusions: The present clinical case aims to show an unusual case of ascending colon volvulus, with initial diagnostic errors; it is intended to inform and instruct medical staff so that they can recognise this presentation of surgical abdomen early, as well as the importance of intervening immediately and avoiding complications.
Introduction
Colonic volvulus is a relatively rare cause of large bowel obstruction, accounting for 10% of colon obstructions (1). It occurs when a loop of bowel rotates on itself and on the mesentery containing the blood vessels that supply its irrigation (2). It is a surgical emergency, as it can lead to intestinal infarction, peritonitis and death if not diagnosed immediately (3). While the diagnosis is clinical, imaging studies can help to pinpoint the location and degree of involvement of the colonic segment prior to surgery and select the appropriate therapeutic approach.
Most volvulus occur in the sigmoid colon (60-80%), cecum (20-40%) and transverse colon (3%); however, any segment of the colon may rotate if it has a long, mobile mesentery that narrows at the base (4). Ascending colon volvulus is a very rare complication of a rare embryological anomaly, characterized by an excessively mobile mesentery (5). Early recognition can prevent disastrous consequences. We present the case of an ascending colon volvulus in a 27-year-old female patient.
Case report
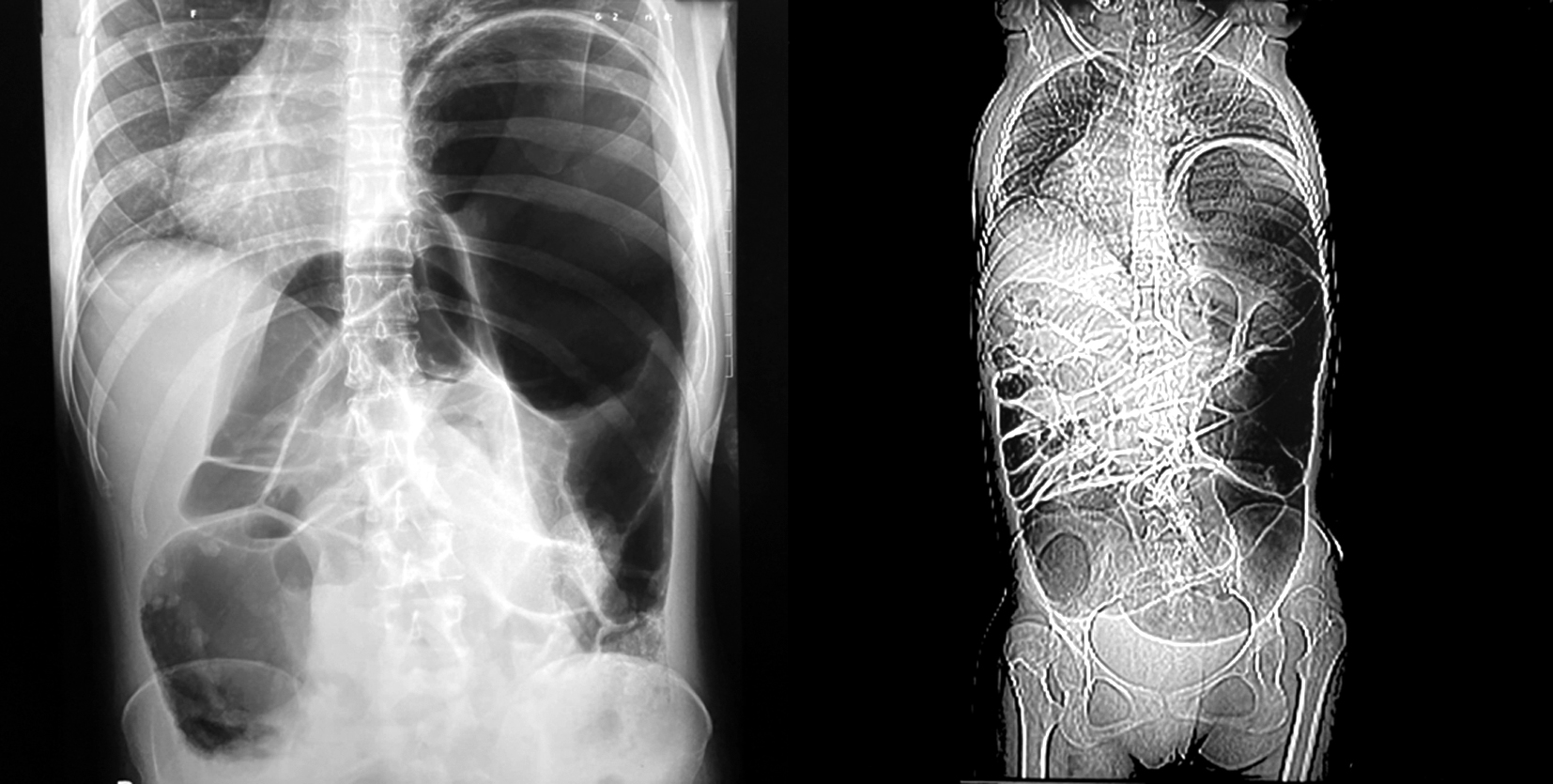
A 27-year-old female patient with a history of sporadic colicky abdominal pain for the last 5 months of mild to moderate intensity, associated with nausea; on some occasions she had to use intravenous anti-spasmodics to relieve the pain. Two days before admission she presented with moderate periumbilical abdominal pain, nausea, vomiting and absence of bowel movements. She was taken to a first level health facility where she underwent a simple abdominal X-ray and reported findings related to intestinal obstruction, as well as a dilated left colonic loop projected towards the left hemithorax associated with displacement of the cardiac silhouette suggestive of diaphragmatic hernia (fig. 1a); for this reason, she was referred to our Hospital.
Among the relevant antecedents is thyroid cancer at the age of 15, for which reason she received treatment with levothyroxine 100 mg once a day orally. On admission she presented BP: 90/60 mmhg, HR: 86 bpm, RR: 18 rpm, Tº: 36.5ºC, SatO2: 92% at FiO2 21%, asthenic patient, dry oral mucous membranes, pale skin ++/+++, Glasgow Coma Scale score: 15 points, with a globular, distended, tympanic abdomen, scarce RHA, soft, depressible, slightly painful on deep palpation. Blood tests showed: Hm: 9770 (02-80-0-0-0-0-18), Ht: 29.6, platelets: 376 000, A+, creatinine: 0.4mg/dl, urea: 20.7, CRP: 22, LDH 252mg/dl, total proteins 7.2g/dl. Gas analysis showed metabolic acidosis. A thoraco-abdomino-pelvic CT scan with contrast (fig. 1b) was performed due to the probability of obstruction secondary to a diaphragmatic hernia according to the radiographic report.
Figure 1 - (a): Plain abdominal radiograph showing a markedly dilated large bowel, predominantly in the upper and left side of the entire abdomen. (b): Panoramic view of the thoracoabdominal-pelvic CT showing a markedly dilated large bowel, starting on the lower right and the entire left side that even elevates the left hemidiaphragm and displaces the heart to the right side.
The CT report concluded: visceral ascension of the left hemidiaphragm, ascites and suspected intestinal obstruction due to sigmoid volvulus (fig. 2 a, b). The patient was scheduled for an emergency laparotomy after resuscitation with crystalloids, intravenous antibiotics, correction of the hydroelectrolyte and acid-base status, transfusion of 01 globular pack to correct the anemia.
Figure 2 - (a): Cross section of the abdominal CT scan at the level of the hepatic dome, showing a very distended colonic segment on the left side. (b): Cross section of the abdominal CT scan at the level of the right upper renal pole, showing a very distended colonic segment predominantly on the left side.

At laparotomy, serous fluid without foul odor was observed within the peritoneal cavity, with a volume of 400cc. A volvulus was found from the ascending colon to the middle third of the transverse colon rotated 180º clockwise, which was causing the obstruction
(fig. 3). There was no gangrene of the intestinal segments involved, but they were very distended and the hepatic flexure of the colon was found to be mobile. The rest of the bowel was normal, the splenic flexure of the colon was found with its normal fixation in the left upper quadrant; the left hemidiaphragm was ascended without the presence of diaphragmatic hernial defects. Right hemicolectomy plus resection of the distal ileum, 10 cm from the ileocecal valve and ileostomy were performed. Subsequently, the cavity was lavaged with 4 litres of tempered sodium chloride. She did not require inotropic support and was extubated in the immediate postoperative period. She went directly to the post-anesthesia recovery unit. Oral tolerance was started at PO1 and feeding was resumed at PO2, and she was discharged on the fourth postoperative day; she was monitored by an outpatient clinic at one week and one month, without incident.
Figure 3 - Intraoperative image showing the volvulus of the cecum, ascending colon and part of the transverse colon rotated on its axis.

Discussion
Obstruction of the large bowel accounts for about 4% of surgical admissions and the causes are diverse, (6) but the most common is colonic neoplasia, which accounts for approximately 60% of cases; other aetiologies include adhesions, diverticulosis, hernia, inflammatory bowel disease and volvulus (7). Although volvulus can occur in other locations in the gastro-intestinal tract, including the stomach, gallbladder and small intestine, it most commonly occurs in the colon (8). In terms of location, it is most common at the level of the sigmoid colon and cecum, being less frequent at the level of the transverse colon, splenic flexure and ascending colon. Sigmoid volvulus is more frequent in adults with chronic constipation and associated neuro-psychiatric disorders, however, cecal volvulus has been reported to be more common in young women (9).
Volvulus of the ascending colon occurs as a result of an abnormality of intestinal fixation resulting in persistence of the mesocolon in the normally retro-peritoneal organ. This is due to intestinal malrotation due to a congenital malformation resulting in an abnormal position of the small and/or large intestine within the peritoneal cavity. Fixation anomalies occur when the midgut does not complete the required 270° counterclockwise rotation during embryological development. Although usually asymptomatic, it can rarely lead to acute colonic obstruction due to volvulus of the ascending colon (10).
According to the production of this process there are three pathophysiological mechanisms: Axial torsion (type 1), where there is a clockwise or counterclockwise rotation on its own longitudinal axis, loop torsion (type 2), where there is a counterclockwise rotation on its longitudinal and transverse axes, and the last, less frequent, cecal scale (type 3), where there is no rotation, folding into the cecum. Types 1 and 2 are the most frequent, accounting for 80% (11).
As for the form of presentation, volvulus should be suspected in those patients with intestinal obstruction associated with abdominal pain and distension, nausea, vomiting, constipation and, on physical examination, a painful abdomen on palpation, distended and tympanic (12). It should also be borne in mind that the presentation is non-specific and varies with the degree of rotation.
The diagnosis of volvulus is primarily clinical. However, in order to confirm the diagnosis, we resort to imaging techniques. Simple radiography is the first line and, together with clinical findings, the diagnosis can be established in up to 60% of cases. However, the imaging study of choice is CT, which allows us to locate the level of obstruction and assess intestinal involvement (S: 100% - E: >90%).(13) Although sometimes the origin of the intestinal obstruction cannot be determined, even in some patients, when the obstructive symptoms worsen, a surgical exploration by laparoscopy or laparotomy is performed, where the definitive diagnosis of the obstruction is finally made. In our patient, despite radiological and tomographic images, there were difficulties in making the diagnosis of ascending colon volvulus, which was confused with sigmoid volvulus and left diaphragmatic hernia.
In terms of management, it is important to consider the hemodynamic status of the patient, as well as the severity, comorbidities and viability of the bowel (14). Detorsion or untwisting, detorsion and cecopexy, cecolopexy or cecostomy, hemicolectomy with colo-stomy and resection with primary ileocolic anastomosis have been described as therapeutic alternatives. While cecostomy and simple detorsion, with or without cecopexy as conservative treatment is a safe procedure with low mortality, a high recurrence rate has been reported. The definitive treatment is right colectomy with primary anastomosis, and bypass with ileostomy and mucosal fistula may be considered in patients with diffuse bowel injury and peritonitis (15).
Conclusions
Colonic volvulus is a group of serious diseases that are difficult to diagnose clinically and involve the same pathophysiological mechanism of rotation. Volvulus of the ascending colon is a rare cause of intestinal occlusion and due to its different forms of clinical presentation, its diagnosis is often complex. Surgical treatment in these patients is the treatment of choice to avoid complications and recurrences.
Scientific contribution
This clinical case shows an intestinal obstruction due to a rare entity, an ascending colon volvulus, a condition that presents a non-specific clinical picture and that despite the help of imaging studies, the preoperative diagnosis can be difficult and, in most cases, the definitive diagnosis is made intraoperatively.
Author’s contributions
José Caballero-Alvarado: conceptualization, research, writing, revision and editing. Mario López-Caballero: drafting, original draft. Carlos Zavaleta: drafting, original draft, editing. Víctor Peralta-Chávez: methodology, review. Katherine Lozano-Peralta: research, review.
Conflicts of interest
The authors declare that they have no conflicts ofinterest.
Funding
Self-financed.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
References
- Bouali M, Yaqine K, Elbakouri A, Bensardi F, Elhattabi K, Fadil A. Ischemicvolvulus of the transverse colon caused by intestinal malrotation: A case report. Int J Surg Case Rep. 2021;83:105971.
2. Le CK, Nahirniak P, Anand S, Cooper W. Volvulus. En: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 [citado 27 de junio de 2022]. Disponible en: http://www.ncbi.nlm.nih.gov/books/ NBK441836/
3. Hasnaoui H, Laytimi F, Elfellah Y, Mouaqit O, Bachir Benjelloun E, Ousadden A, et al. Transverse colon volvulus presenting as bowel obstruction: a case report. J Med Case Reports. 2019;13(1):1-4.
4. Shah R, Klumpp L, Negron-Diaz J, Carmain T, Jordan J, HCA Healthcare/USF Morsani College of Medicine GME Programs at Citrus Memorial Hospital, Inverness, Florida. Transverse colon volvulus in a patient with autism. J Surg Case Rep. 2020;2020(9): rjaa284.
5. Mazingi D, Mbanje C, Muguti GI, Zimunhu T, Mbuwayesango B. Volvulus of the ascending colon due to failure of zygosis: A case report and review of the literature. Int J Surg Case Rep. 2019;59:90-3.
6. Farkas NG, Welman TJP, Ross T, Brown S, Smith JJ, Pawa N. Unusual causes of large bowel obstruction. Curr Probl Surg. 2019; 56(2):49-90.
7. Ramanathan S, Ojili V, Vassa R, Nagar A. Large Bowel Obstruction in the Emergency Department: Imaging Spectrum of Common and Uncommon Causes. J Clin Imaging Sci. 2017;7:15.
8. Ibáñez Sanz L, Borruel Nacenta S, Cano Alonso R, Díez Martínez P, Navallas Irujo M. Vólvulos del tracto gastrointestinal. Diagnóstico y correlación entre radiología simple y tomografía computarizada multidetector. Radiología. 2015;57(1):35-43.
9. Alavi K, Friel CM. Large Bowel Obstruction. En: Steele SR, Hull TL, Read TE, Saclarides TJ, Senagore AJ, Whitlow CB, editores. The ASCRS Textbook of Colon and Rectal Surgery [Internet]. Cham: Springer International Publishing; 2016 [citado 14 de julio de 2022]. p. 669-95. Disponible en: http://link.springer.com/10.1007/978-3-319-25970-3_40
10. Camera L, Calabrese M, Mainenti PP, Masone S, Vecchio WD, Persico G, et al. Volvulus of the ascending colon in a non-rotated midgut: Plain film and MDCT findings. World J Radiol. 2012;4(10): 439-42.
11. López-Cantarero García-Cervantes M, Valdés Hernández I, García Reyes A, Oliva Mompeán F. Bascule or type III cecal volvulus as a rare cause of colonic obstruction. Cir Andal. 2020;31(4):531-3.
12. Rodríguez Fonseca RA, Borge Fajardo L, López Wilson A, Ramos Sánchez D, Cabrera Pérez CR, Fonseca Lloga GM. Vólvulo ceco-ascendente. Rev Nac Itauguá. 2019;102-8.
13. Beyuma-Mora HE, Labastida-Ramírez DL, Vera-Bernal JA, Murguía-Zamora LM, Guevara-Valmaña OI, Beyuma-Mora HE, et al. “Sigma Volvere” acerca del vólvulo de sigmoides, diagnóstico y manejo quirúrgico, reporte de serie de casos. Rev Fac Med México. 2022; 65(2):34-42.
14. Brito Sosa G, Iraizoz Barrios AM. Vólvulo de ciego con lesión de colon ascendente: reporte de un caso y alternativas de tratamiento. Acta Gastroenterológica Latinoam [Internet]. 28 de septiembre de 2021 [citado 15 de julio de 2022];51(3). Disponible en: https://actagastro.org/volvulo-de-ciego-con-lesion-de-colon-ascendente-reporte-de-un-caso-y-alternativas-de-tratamiento/
15. Márquez-Díaz A, Ramírez-Ortega MÁ. Vólvulo de colon derecho con necrosis en paciente joven. Rev Médica Inst Mex Seguro Soc. 2010 [acceso: 10/08/2022];48(2):209-14. Disponible en: https://www. medigraphic.com/cgi-bin/new/resumen.cgi?IDARTICULO=36986
Full Text Sources:
Abstract:
Views: 2922

For Authors
Journal Subscriptions

Sept 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News