Surgery, Gastroenterology and Oncology

|
|
Design: A retrospective case series analysis was conducted to assess clinical outcomes following surgical interventions for patients diagnosed with small bowel carcinomatosis.
Setting: The study was conducted at Chungnam National University Hospital, a tertiary hospital providing specialized oncological care.
Patients and Participants: Thirteen patients with irreversible mechanical small bowel obstruction secondary to stage IV malignant disease were included. Selection was based on confirmed mechanical obstruction via preoperative imaging studies, with interventions performed from January 2013 to December 2022.
Interventions: Surgical procedures included exploratory laparotomy, loop ileostomy, and jejunostomy, tailored to alleviate obstructive symptoms within a palliative framework.
Measurements and Results: Postoperative outcomes were assessed through preoperative imaging findings, surgical procedures, length of hospital stay, and survival times. Eight patients were discharged able to maintain an oral diet. The mean overall survival post-surgery was 78.84 days, with some patients experiencing complications such as recurrent obstruction.
Conclusion: Palliative surgical interventions effectively alleviate obstructive symptoms and improve quality of life for patients with advanced small bowel carcinomatosis. While these procedures provide significant symptomatic relief, the aggressive nature of the malignancy requires ongoing assessment and a multidisciplinary care approach to optimize patient management strategies.
INTRODUCTION
Small bowel carcinomatosis poses a considerable clinical challenge in managing patients with advanced malignancies, particularly due to extensive tumor dissemination within the peritoneal cavity (1). As cancer therapeutics evolve, a growing cohort of patients is experiencing extended survival; however, many endure debilitating obstructive symptoms such as nausea, vomiting, abdominal pain, and constipation, significantly compromising their quality of life (2). These symptoms are indicative of mechanical intestinal failure, necessitating prompt and effective palliative interventions (3).
Palliative surgical approaches have emerged as a viable strategy to alleviate these distressing symptoms, particularly for patients with irreversible mechanical intestinal failure secondary to small bowel carcinomatosis (4). These surgical interventions are critical not only for decompressing the obstructed bowel and redirecting intestinal flow but also for facilitating the resumption of oral intake. Such measures are essential for enhancing patient comfort and optimizing functionality during their remaining lifespan, which directly impacts overall management and survival outcomes (5).
This study seeks to conduct a rigorous analysis of the efficacy and outcomes associated with palliative surgical procedures as part of comprehensive palliative care in addressing the multifaceted obstructive complications of small bowel carcinomatosis. By evaluating clinical outcomes, postoperative recovery, and overall survival, this research aims to provide invaluable insights into how these interventions can positively affect critical care management and inform clinicians in making better decisions regarding the treatment of similar cases in the future.
Methods
Approval was secured from the Institutional Review Board for this retrospective case series, which waived the requirement for informed consent from participating patients. The study focused on 13 patients diagnosed with irreversible mechanical small bowel obstruction secondary to stage IV malignant disease with associated small bowel carcinomatosis, who underwent surgical interventions between January 2013 and December 2022.
Patient selection was predicated on confirmed diagnoses of mechanical obstruction via preoperative imaging studies. The peritoneal carcinomatosis index (PCI) score was calculated based on preoperative computed tomography (CT) findings and operative results, serving as a quantitative metric of the extent of peritoneal involvement by malignant disease within the cohort. Surgical procedures included exploratory laparotomy, with patients undergoing either loop jejunostomy or ileostomy, as deemed clinically appropriate to relieve obstructive symptoms within a palliative care framework.
A comprehensive dataset encompassing clinical and surgical information was collected for each patient to evaluate postoperative outcomes. This included pre-operative imaging findings, surgical procedures performed, and specific variables related to critical care management, such as postoperative recovery processes and the incidence of complications. Additionally, data on length of hospital stay and survival times following surgical intervention were systematically recorded.
This case series aims to delineate the clinical outcomes and experiences associated with palliative surgical procedures in this patient cohort, contributing insights that may assist in managing similar cases in clinical practice, particularly emphasizing the impact of these interventions on the overall critical care management of patients suffering from small bowel carcinomatosis.
RESULTS
A total of 13 patients were identified with irreversible mechanical small bowel obstruction due to stage IV malignant disease associated with small bowel carcinomatosis. The clinical characteristics of the patient cohort are detailed in table 1.
Table 1 - Clinical Characteristics
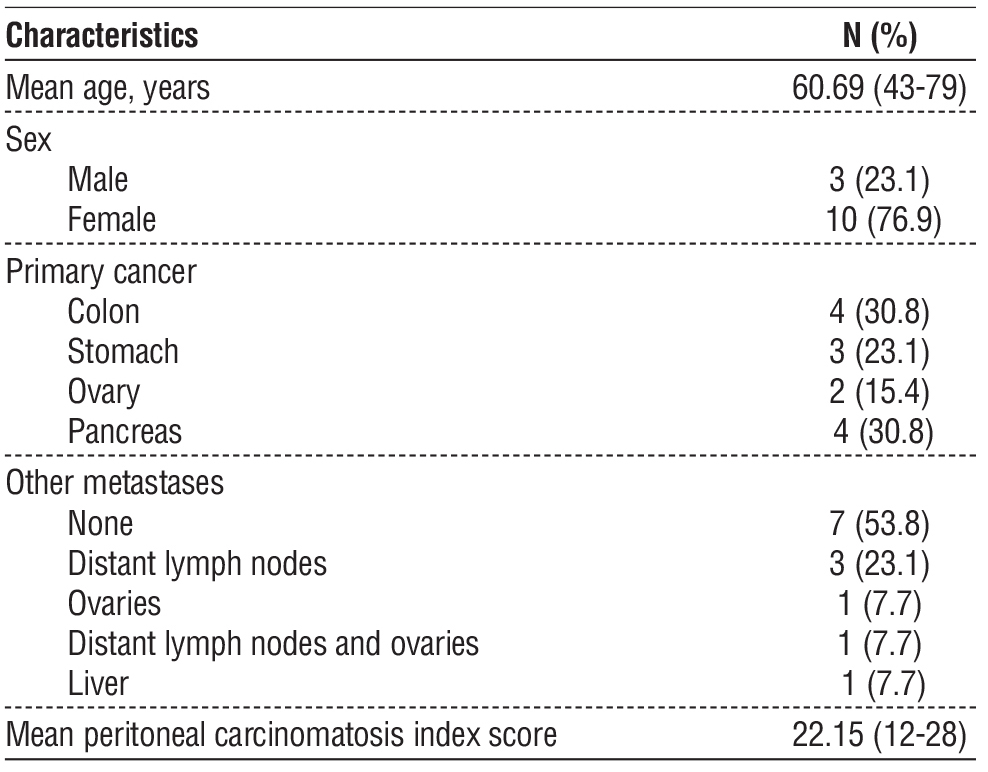
The mean peritoneal carcinomatosis index (PCI) score was 22.15, with a range from 12 to 28, indicating a substantial disease burden among patients and serving as a critical prognostic indicator for outcomes in this population.
Surgical characteristics and outcomes are summarized in table 2. The majority of interventions performed were ileostomy procedures, effectively addressing obstructive symptoms. Specifically, eight patients underwent successful loop ileostomy at the terminal ileum. In contrast, two patients required jejunostomy due to anatomical constraints that precluded ileostomy. One patient was treated with a bypass enteroenterotomy and ileostomy, while another underwent segmental resection of the small bowel, followed by ileostomy. Additionally, one complex case necessitated both jejunostomy and ileostomy to decompress a closed-loop obstruction of the ileum.
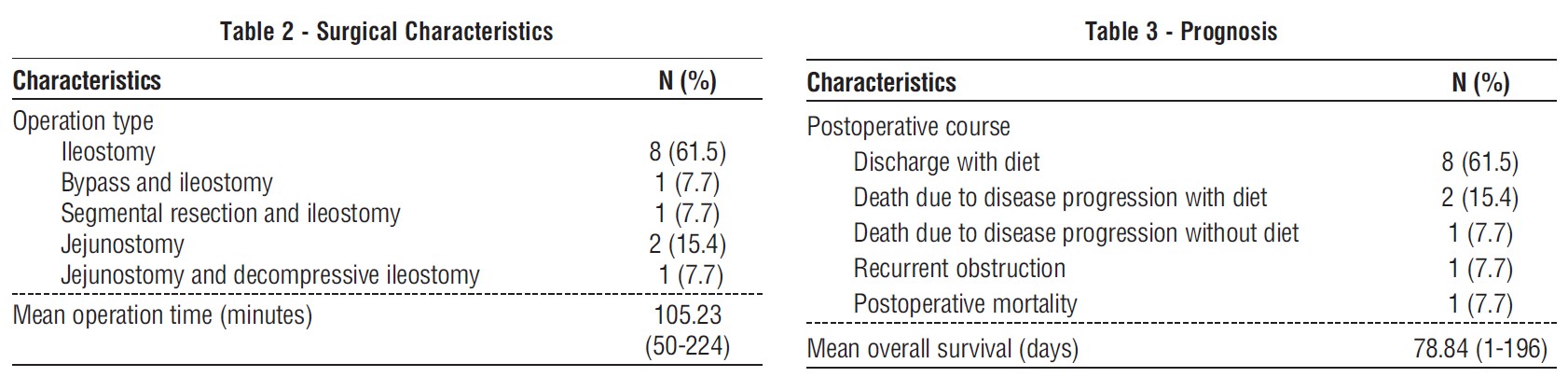
Postoperative outcomes and prognostic information are further detailed in table 3. Eight patients were discharged with the ability to maintain an oral diet, indicating immediate functional improvement and positive outcomes post-surgery. The analysis of recovery rates revealed that while most patients experienced symptomatic relief, the clinical trajectories were complicated; two patients succumbed to progressive disease shortly postoperatively. One patient experienced recurrent obstruction on post-operative day 12, necessitating readmission for evaluation and possible intervention. Furthermore, two patients exhibited exacerbated health deterioration in the immediate postoperative period, underscoring the precarious nature of their prognoses.
Survival analysis revealed a mean overall survival of 78.84 days following palliative surgery, with a range from 1 day to 196 days. This variability in survival illustrates the intricate interplay between surgical outcomes, individualized patient factors, and the aggressive nature of disease progression. Collectively, the outcomes highlight that while palliative surgeries can provide significant symptomatic relief and facilitate dietary intake, the aggressive behavior of the underlying malignancy considerably impacts both short- and long-term patient outcomes. This underscores the importance of thorough postoperative monitoring and management within the context of critical care in these complex cases.
DISCUSSION
Palliative surgical intervention is pivotal in managing patients with irreversible mechanical intestinal failure due to small bowel carcinomatosis (1). The procedures executed within this cohort effectively alleviated obstructive symptoms, significantly enhancing patients' quality of life and facilitating the resumption of oral intake (7). Such enhancements are critical for maintaining nutritional status and overall well-being during end-of-life care, particularly for those confronted with advanced malignancies (8).
The challenges associated with irreversible intestinal failure, especially in the context of small bowel carcinomatosis, arise from the aggressive pathology of these malignancies and their complications (1). Patients in this cohort typically present with a complex clinical profile characterized by systemic disease progression, impaired bowel function, and severe malnutrition (7). Given these factors, the primary objective of palliative surgical interventions should be to focus on symptom relief and improve quality of life, rather than pursuing curative intent (9).
In this case series, the majority of patients underwent loop ileostomy, enabling effective bowel decompression. This reflects the necessity to divert intestinal contents and alleviate obstructive symptoms (7). While the benefits of such procedures are evident, it is essential to acknowledge the inherent risks, including postoperative complications that may adversely affect outcomes (10). Although most patients successfully maintained an oral diet following surgery, a subset experienced significant complications, such as recurrent obstruction and deterioration of overall health (6).
The mean survival duration of 78.84 days following surgery underscores the precarious nature of managing patients with stage IV malignancies. This finding aligns with existing literature, which often illustrates immediate symptomatic relief while highlighting the rapid progression of underlying disease processes (7). The urgent need for a multidisciplinary approach emerges, integrating palliative care principles with surgical interventions (10). Collaboration among surgeons, medical oncologists, and palliative care specialists is critical for optimizing patient outcomes and ensuring comprehensive care that addresses both physical and psychosocial aspects of terminal illness (11).
Furthermore, the average peritoneal carcinomatosis index score of 22.15 in our cohort serves as a vital prognostic metric that informs decision-making regarding surgical interventions. This scoring system reflects the extent of peritoneal involvement and provides insights into potential surgical outcomes and the likelihood of successful symptom management. Higher scores are associated with poorer survival; therefore, the palliative benefits of surgery should be evaluated individually, particularly in a patient population where quality of life is paramount (12-15).
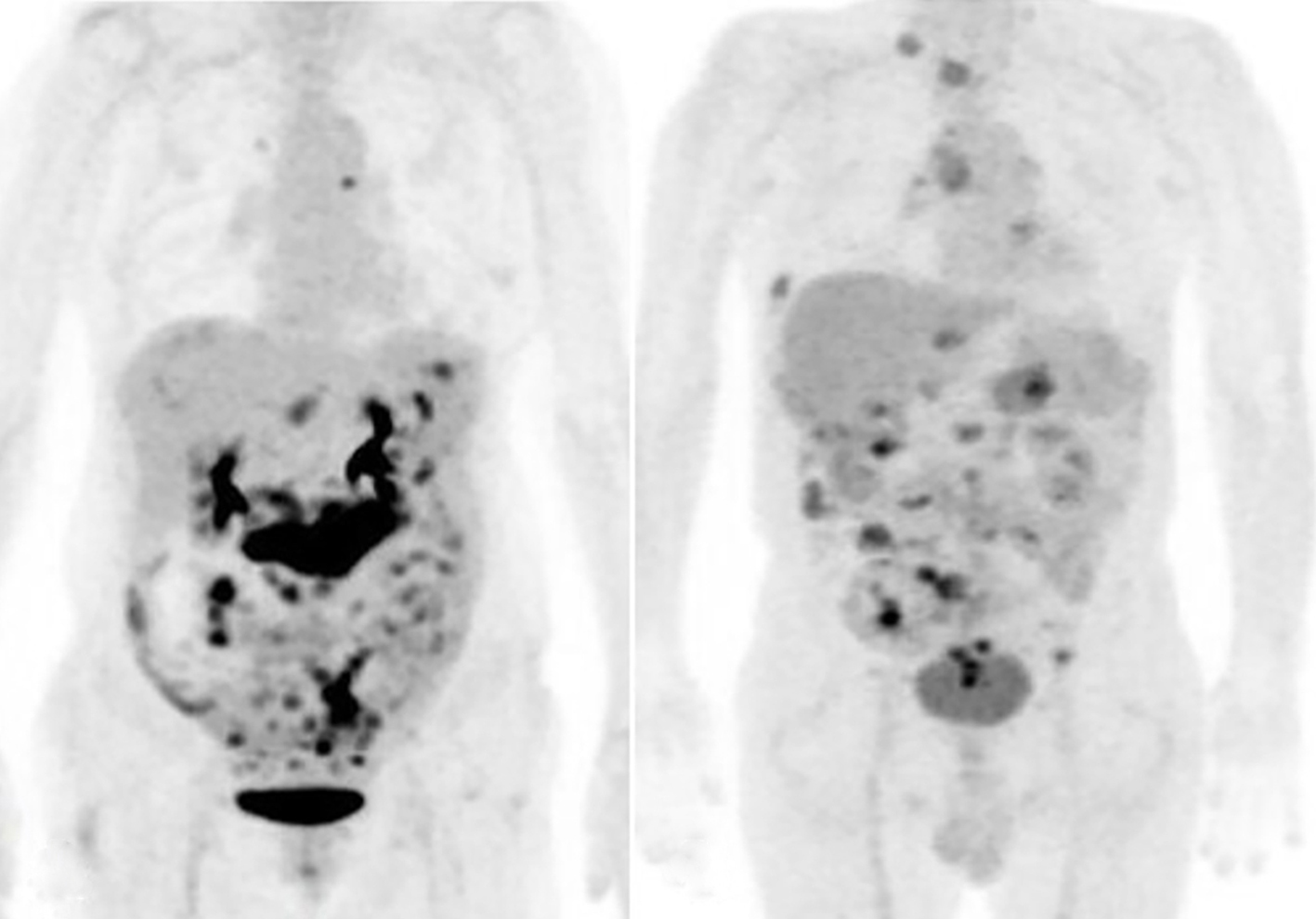
Importantly, preoperative imaging plays a crucial role in understanding disease extent and informing
surgical strategies. Future studies should compare the outcomes of advanced imaging modalities, such as MRI or PET scans, with conventional CT to provide a more comprehensive evaluation of disease burden and anatomical complexities (16-19). The relatively high PCI scores observed in our study suggest that, despite the challenges, palliative surgery can facilitate the maintenance of dietary intake throughout overall survival, enhancing quality of life during patients' remaining lifespan (fig. 1).
Figure 1 - PET scans shows high PCI scores (a) Case 7 with 27 PCI score; (b) Case 10 with 23 PCI score
In considering the impact of palliative surgery on critical care management, it is vital to recognize the limitations of this study, including its retrospective design and small sample size, which may restrict the generalizability of the findings. Additionally, the single-institution focus may introduce biases related to local practices and patient demographics. Future research efforts should aim to involve larger, multicenter cohorts to validate these findings and explore the efficacy of various surgical strategies in diverse patient populations, as well as deepen the understanding of how these interventions can improve overall management and outcomes in critically ill patients.
CONCLUSION
Palliative surgery plays a critical role in the management of obstructive symptoms in patients with irreversible intestinal failure due to small bowel carcinomatosis. These surgical interventions not only alleviate distress but also facilitate the resumption of oral intake, significantly enhancing the quality of life for this vulnerable patient population. However, while palliative surgery provides symptomatic relief, it is essential to recognize that the aggressive progression of malignancy can limit the duration and extent of these benefits.
As such, ongoing patient assessment and a multi-disciplinary care approach are necessary to optimize outcomes in patients facing complex challenges in their treatment pathways. The integration of surgical care with comprehensive palliative strategies is vital for addressing both the physical and psychosocial aspects of terminal illness, ultimately improving the quality of care within the realm of critical patient management. This study highlights the importance of such multi-disciplinary collaboration in enhancing outcomes and quality of life in patients with advanced malignancies.
Acknowledgments
We would like to express our heartfelt gratitude to our fellow alumni from the Department of Surgery at Chungnam National University Hospital for their invaluable support and encouragement throughout this study. Your contributions have greatly enriched our research experience.
Author’s Contributions
KH Lee: the acquisition of data, analysis and interpretation of the data, and drafting of the manuscript. Y Sul: study conception and design, acquisition of data, and critical revision of the manuscript
Conflict of Interests
The authors declare that there is no conflict of interest.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial, or not-
for-profit sectors.
Data Availability Statement
The datasets and analysis during the current study are available from the corresponding author on reasonable request.
REFERENCES
1. Ripamonti CI, Easson AM. Management of malignant bowel obstruction. Eur J Cancer. 2008;44(8):1105–15.
2. Blair SL, Chu DZJ, Schwarz RE. Outcome of palliative operations for malignant bowel obstruction in patients with peritoneal carcinomatosis from nongynecological cancer. Ann Surg Oncol. 2001;8(8):632–7.
3. Miner TJ, Jaques DP, Shriver CD. A prospective evaluation of patients undergoing surgery for the palliation of an advanced malignancy. Ann Surg Oncol. 2002;9(7):696–703.
4. Helyer L, Easson AM. Surgical approaches to malignant bowel obstruction. J Support Oncol. 2008;6(3):105–13.
5. Krouse RS, McCahill LE, Easson AM, Dunn GP. When the sun can set on an unoperated bowel obstruction: management of malignant bowel obstruction. J Am Coll Surg. 2002;195(1):117–28.
6. Podnos YD, Juarez G, Pameijer C, Uman G, Ferrel BR, Wagman LD. Surgical palliation of advanced gastrointestinal tumors. J Palliat Med. 2007;10(4):871–6.
7. Gwilliam B, Bailey C. The nature of terminal malignant bowel obstruction and its impact on patients with advanced cancer. Int J Palliat Nurs. 2001;7(10):474–81.
8. Soriano A, Davis MP. Malignant bowel obstruction: individualized treatment near the end of life. Cleve Clin J Med. 2011;78(3): 197–206.
9. Ripamonti CI, Twycross R, Baines M, Bozzetti F, Capri S, De Conno F, et al. Clinical-practice recommendations for the management of bowel obstruction in patients with end-stage cancer. Support Care Cancer. 2001; 9(4):223–33.
10. Selby D, Wright F, Stilos K, Daines P, Moravan V, Gill A, et al. Room for improvement? A quality-of-life assessment in patients with malignant bowel obstruction. Palliat Med. 2010;24(1):38-45.
11. Abbott SM, Merrie AE. Resection of peritoneal metastases causing malignant small bowel obstruction. World J Surg Oncol. 2007;5(1): 122–5.
12. Huang Y, Alzahrani NA, Chua TC, Liauw W, Morris DL. Impacts of low peritoneal cancer index on the survival outcomes of patients with peritoneal carcinomatosis of colorectal origin. Int J Surg. 2015; 23(Pt A):181-5.
13. Chan CHF, Cusack JC, Ryan DP. A critical look at local-regional management of peritoneal metastasis. Hematol Oncol Clin North Am. 2015;29(1):153-8.
14. de Boer NL, Brandt-Kerkhof ARM, Madsen EV, Doukas M, Verhoef C, Burger JWA. The accuracy of the surgical peritoneal cancer index in patients with peritoneal metastases of colorectal cancer. Dig Surg. 2021;38(3):205-11.
15. Salo SAS, Lantto E, Robinson E, Myllärniemi M, Laaksonen S, Salo JA, et al. Prognostic role of radiological peritoneal cancer index in malignant peritoneal mesothelioma: national cohort study. Sci Rep. 2020;10(1):13257.
16. Reginelli A, Giacobbe G, Del Canto MT, Alessandrella M, Balestrucci G, Urraro F, et al. Peritoneal carcinosis: what the radiologist needs to know. Diagnostics (Basel). 2023;13(11):1974.
17. Lee RM, Zaidi MY, Gamboa AC, Speegle S, Kimbrough CW, Cloyd JM, et al. What is the optimal preoperative imaging modality for assessing peritoneal cancer index? An analysis from the United States HIPEC collaborative. Clin Colorectal Cancer. 2020;19(1):e1-e7.
18. Panagiotopoulou PB, Courcoutsakis N, Tentes A, Prassopoulos P. CT imaging of peritoneal carcinomatosis with surgical correlation: a pictorial review. Insights Imaging. 2021;12(1):168.
19. van 't Sant I, Engbersen MP, Bhairosing PA, Lambregts DMJ, Beets-Tan RGH, van Driel WJ, et al. Diagnostic performance of imaging for the detection of peritoneal metastases: a meta-analysis. Eur Radiol. 2020;30(6):3101-12.
Full Text Sources:
Abstract:
Views: 883

For Authors
Journal Subscriptions

Jun 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News