Surgery, Gastroenterology and Oncology

|
|
Purpose: Failure and recurrence are concerns in nonoperative management (NOM) for acute appendicitis (AA) and interval appendectomy (IA). The goal of the study was to identify predictors of failure and recurrence in patients with AA who underwent NOM.
Methods: A total of 348 adults with appendicitis were treated in our department from April 2016 to October 2021. Among these patients, 337 who did not undergo emergency surgery were divided into those for whom NOM was unsuccessful, leading to unplanned surgery (n=28) and those successful with NOM (n=309). These groups were compared to identify predictive factors for NOM failure. In the NOM-success group, 195 patients were further subdivided into non-recurrence (n=166) and recurrence (n=29) groups to identify predictive factors for recurrence of appendicitis.
Results: In multivariate analysis, posttreatment CRP level [odds ratio (OR) = 1.126, 95% onfidence interval (CI) 1.076-1.179, P < 0.001] and fecal stones with abscess formation (OR=5.530, 95% CI 2.081-14.691, P=0.001) were independently associated with NOM failure. Receiver operating characteristic curve analysis showed an optimum cutoff CRP level of 10.46 mg/dl for appendicitis treatment failure. The initial CRP level was significantly lower and the percent drop of CRP was significantly higher in the recurrence group than in the non-recurrence group.
Conclusions: These findings suggest that the posttreatment CRP level and fecal stones with abscess formation are predictors for NOM failure, but that recurrence may not be affected by the severity of previous bouts of appendicitis.
Abbreviations: NOM: nonoperative management; AA: acute appendicitis; IA: interval appendectomy; OR: odds ratio; CI: confidence interval; UA: unplanned appendectomy.
Introduction
Acute appendicitis (AA) is a common gastroenterological disease that often requires urgent surgery. However, nonoperative management (NOM) for children with uncomplicated AA appears to be effective based on less morbidity, fewer disability days, and lower costs compared to surgery (1,2). There are also reports of NOM for uncomplicated AA in adults, mitigating the need for an appendectomy (3-5). However, failure of NOM is a concern in both pediatric and adult patients, with failure rates of 8.5-10% in patients with uncomplicated appendicitis (5-7), an increased failure risk in patients with an appendicoliths (6), and failure in complicated appendicitis involving abscess formation or perforation. Thus, there is a need to identify patients at high risk for NOM failure to avoid taking unnecessary risks with such patients.
After NOM for appendicitis, it is important to consider whether patients should undergo an interval appendectomy (IA). One concern with IA is recurrence after NOM, since a recent meta-analysis found the recurrence rate of symptoms within one year to be 27.4% (8). Nonetheless, this also indicates that about 70% of adult patients do not experience recurrent appendicitis after NOM. Therefore, careful screening to select patients with a low risk of AA recurrence or need for IA could avoid unnecessary surgery (9). We usually treat AA cases with NOM, with the exception of those with diffuse peritonitis or severe conditions such as septic shock, disseminated intravascular coagulopathy, or refractory pain control. We then perform IA on appendicitis cases with fecal stones or abscess formation, as well as recurrence cases. Herein, we have analyzed short-term outcomes of IA, risk factors for NOM failure, and recurrence after NOM to evaluate the feasibility of NOM in adult patients with AA.
Materials and Methods
Patients
Following approval by the system’s institutional review board, a retrospective analysis was performed on 348 adult patients with AA who were treated at Aomori City Hospital from April 2016 to October 2021. Of these patients, 11 underwent emergency appendectomy and 337 were initially treated with NOM. Among the NOM cases, 309 cases were successful and patients were discharged (NOM-success group), whereas abdominal or general conditions deteriorated in 28 patients, and an unplanned appendectomy (UA) was performed (NOM-failure group).
Analysis of recurrence was performed oin the 300 patients on the NOM-success group, after excluding six patients diagnosed with appendix or cecum cancer and the three patients who opted to undergo surgery at other institutions. Elective IA was recommended for patients with recurrence, and those for whom a fecal stone or abscess formation was detected in the clinical course. A total of 105 patients initially underwent IA. No further treatment was performed at the outset, for 195 patients, 166 of whom had no recurrence (non-recurrence group). In 29, recurrent appendicitis (recurrence group) occurred, and they subsequently underwent additional NOM. Recurrence was defined as a diagnosis of AA after initial treatment and rehospitalization that required treatment, regardless of the period of time that elapsed prior to recurrence.
NOM failed in one patient in the recurrence group and UA was performed. NOM was successful in the other 28 patients with recurrence, 16 of whom underwent subsequent IA, while 12 patients refused IA. In total, 150 patients were treated with appendectomy (excluding emergency appendectomy), including 121 who underwent IA (IA group), and 29 who underwent UA (UA group) (fig. 1).
Figure 1 - Flow diagram for the disposition of 348 patients who underwent treatment for appendicitis between April 2016 and October 2021

Diagnosis of appendicitis
A diagnosis of appendicitis was based on typical clinical symptoms, such as elevated body temperature, nausea, anorexia, abdominal pain, tenderness in the right lower quadrant, and inflammation in laboratory findings. A contrast CT scan was also routinely performed, and appendicitis was diagnosed if any of the following were found: appendiceal dilatation > 5 mm, wall thickening or enhancement, or periappendiceal fat stranding. Cases were also divided into what were considered uncomplicated and complicated types, with the definition of complicated appendicitis being based on the presence of an appendicolith or abscess formation.
Nonoperative management protocol
All patients were started off by withholding of food, giving intravenous fluid support, and administering cefmetazole or piperacillin/tazobactam, with the addition of metronidazole in cases with abscess formation. Clinical condition, mainly including abdominal findings, were evaluated twice daily, and blood tests were usually performed on hospital days 1 and 3. If the patient did not improve without diffuse peritonitis, treatment was changed by the addition of, or a switch to, more broad-spectrum antibiotics, such as meropenem. If conditions worsened despite the change of antibiotics, an urgent appendectomy was performed. Patients with a good clinical response to antibiotic therapy, as proven by adequate enteral intake, were discharged. IA was recommended for patients with fecal stones or abscess formation, and those with post-discharge recurrence, who were instructed to return to the hospital.
Statistical analysis
Continuous variables are expressed as medians and have been compared using the Mann-Whitney U test. Categorical variables were compared using the Pearson Chi-square test with a Fisher exact test, where appropriate, in univariate analysis. Multivariate logistic regression analysis was performed using variables that were significant in univariate analysis. Receiver operating characteristic (ROC) curve analysis was used to determine the cutoff for each extracted risk factor, and then the sensitivity and specificity were calculated. All statistical analyses were performed using SPSS for Windows/MacTM ver.25.0 (SPSS Inc., Chicago, IL, USA). Significance was defined at the 5% level.
Results
Safety of an interval appendectomy (IA)
The surgical outcomes in the IA and UA groups are shown in table 1. Laparoscopic approaches were used in 123 patients overall (82.0%), and significantly more frequently in the IA group compared to the UA group (97.5% (113/121) vs. 17.2% (5/29), p < 0.001). The overall conversion rate to open surgery was 5.7% (7/123), and was significantly lower in the IA group (4.2% (5/118) vs. 40% (2/5), p = 0.026). The median operation time was 73.0 (range, 26-262) min and the median blood loss was 2.0 (2-938) ml, both of which were significantly lower in the IA group (70.0 vs. 102.0 min, p = 0.008; 2.0 vs. 40.0 ml, p < 0.001). The overall postoperative complication rate was 10% (15/150) and was also significantly lower in the IA group (3.3% (4/121) vs. 37.9% (11/29), p < 0.001). Complications of Clavien-Dindo grade ≥ IIIa (10), all of which were residual abscesses, were found in a total of three patients (2.0%), including one in the IA group and two in the UA group (0.8% (1/121) vs. 6.9% (2/29), p = 0.096). The median postoperative hospital stay was 4 (1-35) days and was significantly shorter in the IA group (3 (1-18) vs. 13 (3-35) days, p < 0.001).
Table 1

Risk factors for NOM failure
The characteristics of the 337 patients (186 males, 151 females) are summarized in table 2. The NOM failure rate was 8.3%. The median age was 47.0 (16-93) years. The ASA-PS (American Society of Anesthesiologists Physical Status) was one in 68 patients (20.2%), two in 230 (68.2%), and three in 39 (11.6%). There was no significant difference in gender, age, or ASA-PS between the NOM-success and the NOM-failure groups. For all patients, the median initial white blood cell (WBC) count was 12,695 (1,380-24,800) /µL, and the posttreatment WBC count was 6,450 (1,400-25,000) /µL; the initial C-reactive protein (CRP) level was 3.45 (0.02-48.8) mg/dl, and the posttreatment CRP level was 4.69 (0.04-48.95) mg/dl. The median percentages of decrease (posttreatment/initial × 100) were 57.1% (11.7-623.2%) for WBC count and 126.3% (4.1-71,300.0%) for CRP.
Table 2

The NOM-failure group had significantly higher initial CRP levels (6.87 (0.06-34.19) mg/dl, p = 0.001), posttreatment WBC count (9,600 (3,760-19,870) mg/dl, p < 0.001), and posttreatment CRP levels (20.39 (2.31-48.95) mg/dl, p=0.000) compared with the NOM-success group. The percentages of decrease in WBC count (83.4% (35.3-285.3%), p < 0.001) and CRP (212.0% (49.6-12,750.0%), p = 0.039) were significantly higher in the NOM-failure group.
CT imaging showed overall rates of fecal stones of 45.4% (153/337), abscess formation at 25.8% (87/337), and both fecal stones and abscess formation of 12.5% (42/337), and each rate was significantly higher in the NOM-failure group (75.0% vs 42.7%, p = 0.001; 67.9% vs 22.0%, p < 0.001; 50.0% vs 9.1%, p < 0.001, respectively). The median appendix diameter was 11 (5-30) mm, and the appendix was significantly more dilated in the NOM-failure group (14 mm (8-20 mm), p = 0.000).
In multivariate analysis, the posttreatment CRP level (odds ratio (OR) = 1.126, 95% confidence interval (CI) 1.076-1.179, p < 0.001) and the presence of fecal stones and abscess formation (OR = 5.530, 95% CI 2.081-14.691, p = 0.001) were independently associated with NOM failure (table 3). ROC curve analysis showed that the optimum cut-off CRP level for NOM failure was 10.46 mg/dl, with 74.1% sensitivity, 74.0% specificity, and the AUC was 0.848 (95% CI 0.781-0.916, P < 0.001; fig. 2).
Table 3

Figure 2 - Receiver operating characteristic (ROC) curves of the relationship of the C-reactive protein (CRP) level with NOM failure

Malignant lesions
Appendiceal tumors, including low-grade appendiceal neoplasms (LAMN), and colon cancers (cecum and ascending colon) were identified in 2.6% (9/348) of cases. Of the 309 patients in the NOM-success group, six (1.9%) were diagnosed with malignancy after NOM and then underwent ileocecal resection or right hemicolectomy for cancer. In three patients, a malignant lesion was detected pathologically after IA. Two LAMN cases were kept under observation without additional surgery. One patient was diagnosed with appendix cancer after appendectomy and underwent a subsequent ileocecal resection.
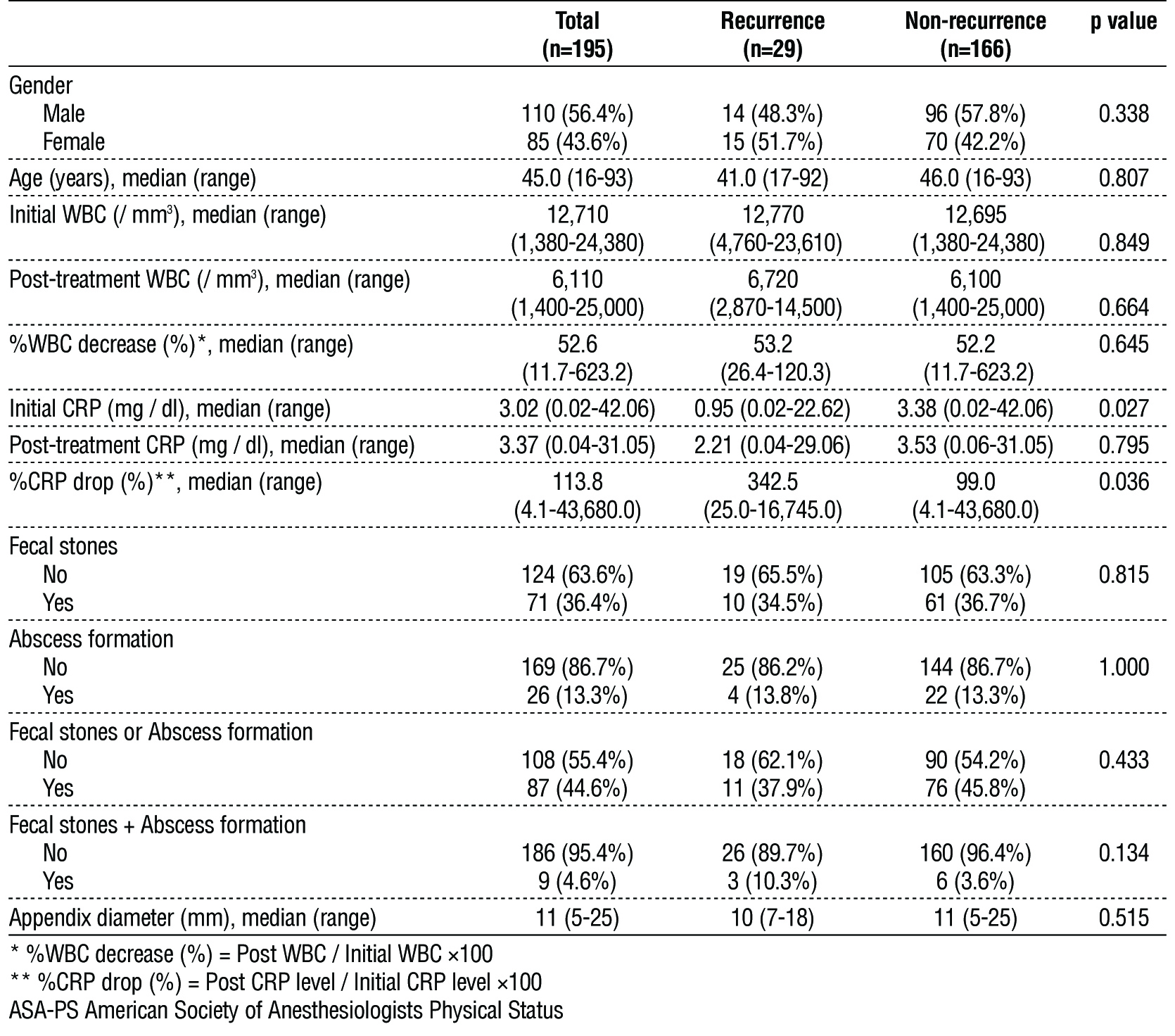
Risk factors for recurrence
The recurrence rate was 14.9% and the median age in recurrence cases was 45.0 (range 16-93) in the patients in the recurrence and non-recurrence groups (table 4). There was no significant difference in gender or age between these groups. In these patients, the median initial WBC count was 12,710 (1,380-24,800) /µL, the posttreatment WBC count was 6,110 (1,400-25,000) /µL, the initial CRP level was 3.02 (0.02-42.06) mg/dl, and the posttreatment CRP level was 3.37 (0.04-31.05) mg/dl. The median percent of decreases of WBC count and CRP were 52.6% (11.7-623.2%) and 113.8% (4.1-43,680.0%), respectively. The initial CRP level in the recurrence group (0.95 (0.02-22.62) mg/dl, p = 0.001) was significantly lower and the percent of decrease of CRP (342.5% (25.0-16,745.0%), p = 0.039) was significantly higher than those in the non-recurrence group. No other parameters differed significantly between the two groups, including the presence of fecal stones, abscess formation, both fecal stones and abscess formation, or appendix diameter on CT.
Table 4
Discussion
This study investigated the feasibility of NOM for uncomplicated and complicated appendicitis, and the outcomes of IA for high-risk patients. The results showed differences between the IA and UA groups, NOM-success and NOM-failure groups, and recurrence and non-recurrence groups, with three main results. First, the short-term surgical outcomes, operation time, blood loss, complication rate, and postoperative hospital stay were significantly better in the IA group than in the UA group. Second, posttreatment CRP level, as well as fecal stones and abscess formation were independent risk factors for NOM failure. Finally, the initial CRP level was significantly lower and the percentage of decrease in CRP was significantly higher in the recurrence group than in the non-recurrence group.
The feasibility of NOM and subsequent IA remains controversial in terms of morbidity, efficacy, recurrence, and cost. In 2021, a Japanese nationwide study showed that emergency surgery for complicated AA places the patient at relatively higher risk, while the risk associated with an elective appendectomy is significantly lower than that of other methods (11). A systematic review and meta-analysis showed that immediate surgery is associated with higher morbidity than nonsurgical treatment (12), and another meta-analysis suggested that, for both uncomplicated and complicated adult AA, NOM with antibiotics was associated with significantly fewer complications and a shorter hospital stay (13). Thus, the benefits of NOM and IA seem to be safer surgery with lower complication rates, as also reflected in the authors’ results.
Nevertheless, there are reports that indicate concerns with NOM, including one of the above-mentioned studies, showing lower efficacy and higher relapse with NOM compared to an appendectomy (13). An open-label randomized controlled trial in patients with AA in 2007 demonstrated that amoxicillin plus clavulanic acid was non-inferior to emergency appendectomy based on rates of 30-day postintervention peritonitis, unplanned appendectomy, and recurrence (14). A retrospective study of 1081 patients who underwent appendectomy for AA in 2006 showed that an immediate appendectomy is the necessary course of action based on the risk of developing advanced pathologies, and, that postoperative complications increase with time (15). However, these two studies were performed more than ten years ago and modern conservative treatment strategies, including new antibiotics, may be more effective.
One advantage of NOM is the potential to explore the possibility of malignancies after NOM. This institution routinely performs a total colonoscopy after NOM for patients > 40 years old, and appendiceal tumors or colon cancers have been discovered in 1.9% (6/309) of successful NOM cases, with 2.5% (3/121) diagnosed incidentally after IA. A retrospective review of IA for complicated appendicitis in 402 patients found a 9% rate of appendiceal neoplasms, with this rate rising to 11% in patients ≥ 30 years old, and 16% in patients ≥ 50 years old (16). Other reports have shown rates of 10-29%, (17-21) but the neoplasm rate in patients with complicated appendicitis is thought to be higher (17,19,22). Therefore, from an oncological perspective, complicated appendicitis, such as cases with abscess or mass formation, may be better treated as conservatively as possible. NOM and subsequent total colonoscopy are helpful in cancer surgery with complete lymph node dissection for possible appendix or colon cancer.
Regarding NOM for appendicitis, including complicated appendicitis, the two main concerns are failure and recurrence. A randomized controlled study suggested that fever at initial presentation, presentation with elevated serum CRP, or an intraluminal fecalith were risk factors for NOM failure (14). Another retrospective study showed that the combination of elevated CRP and a fecalith predicted failure of antibiotic therapy in 224 patients who received antibiotics initially (23). From a radiological perspective, in a retrospective study, (24) incarceration of an appendicolith and periappendiceal fluid on CT images were suggested to be predictive factors for failure of NOM. In this study, the posttreatment CRP level and abscess formation with a fecalith were identified as independent risk factors for failure of NOM; the combination of the presence of a fecalith and abscess formation, in particular, resulted in extremely high odds for NOM failure.
The recurrence rate of AA has been reported as 14-35%, (8,14,25,26) and recurrence risk factors have been identified in several studies. In 2000, a retrospective study in 60 patients with appendicitis suggested an appendix diameter of > 8 mm measured through ultrasonography indicated a risk for recurrence (27). Recently, a retrospective study of 12,235 patients who underwent NOM for appendicitis found, in multivariate analysis, that recurrence was independently associated with young age, male gender, percutaneous abscess drainage, and medical center admission (28). An initial CRP level > 10.3 mg/dl was found to be an independent risk factor for recurrence of appendicitis in children with appendiceal masses in a retrospective study conducted in 2017 (29). However, the results of this study suggest that initial CRP levels in the recurrence group were significantly lower than those in the non-recurrence group, and that the percentage drop of CRP was higher in the recurrence group.
Good surgical outcomes were obtained in patients who underwent IA. This may be due to stable overall conditions, good vital signs, and a low level of inflammation in the IA group. Conversely, in the UA group, intense bacteremia due to severe appendicitis leading to possible abscess formation, or perforation, or even peritonitis may make surgery challenging both intra- and postoperatively. Emergency appendectomy is technically demanding due to distorted anatomy, bowel adhesive loops, and difficulty closing the appendiceal stump due to inflamed tissues (30). Under such conditions, early laparoscopic appendectomy for AA may be converted to open appendectomy, ileocecal resection, or right hemicolectomy, (31) as found in this study. There may also be complications postoperatively, including infection and organ failure. Emergency surgery should be avoided whenever possible because of these intra- and postoperative difficulties, but conservative treatment also has a risk for mortality.
We found that that the posttreatment CRP level and a combination of fecal stones and abscess formation were associated with NOM failure. CRP is broadly known as a marker that indicates an inflammatory response, and the posttreatment CRP level reflects overall inflammation severity and response to antibiotics. The percentage drop of CRP was not a significant factor in multivariate analysis, which may be due to the insufficient effect of antibiotics due to severe inflammation or a result of raising the CRP level too late. The presence of abscess formation may also reflect the intensity of inflammation, and there is a need to consider the relationship between fecal stones and inflammation severity, as well as the location and size of the stones. As mentioned above, incarceration of fecal stones has been suggested to be an independent risk factor for NOM failure, (24) and such incarceration may exacerbate inflammation.
This study showed that the initial CRP level was significantly lower and the percentage drop of CRP was significantly higher in the recurrence group than in the non-recurrence group. These results are challenging to interpret because the recurrence rate has been found to increase with more severe inflammation in initial appendicitis in other reports (28,29). However, in the event of a low initial CRP level and a high rate of percentage drop of CRP after antimicrobial therapy, resistance to treatment with antimicrobials or an individual's potential weak resistance to inflammation may be reflected. With such inference the patient is more likely to develop appendicitis for the second time or experience subsequent inflammation. The results of this study suggest that the severity of initial appendicitis may not be related to recurrence. However, the greater the percentage drop of CRP is might suggest that patients with recurrence are more vulnerable to infection, including appendicitis. Other factors that may be associated with recurrence include microbiota, (32) daily bowel movement issues, (33) and specific morphological characteristics of the appendix (34).
In the present study, posttreatment CRP level and fecal stones with abscess formation after conservative treatment were significant risk factors for NOM failure. Although it was mentioned earlier that the surgical outcome of IA after conservative treatment is favorable, it is desirable to perform early surgery in cases with the two aforementioned risk factors, considering the deterioration of the general condition, the occurrence of surgical and systemic complications, and the risk to life due to NOM failure. Keeping in mind that straightforward continuation of conservative treatment may lead to treatment failure, it is crucial to avoid missing the appropriate timing for surgery. On the other hand, although no significant difference was observed in the multivariate analysis in this study, it can be inferred that early IA should be considered for patients with low initial CRP levels and a high percentage drop of CRP at initial presentation as that puts patients in a high-risk group for recurrence even after the first onset, although this does deviate from the usual protocol.
This study has several limitations, including the small number of patients and the retrospective, non-randomized design without a control group. Also, a standard definition of complicated appendicitis has not been established and target cases differ among studies, which makes it difficult to compare the present results with those from previous studies.
In conclusion, the posttreatment CRP level and fecal stones with abscess formation may be predictors of NOM failure. However, recurrence of appendicitis does not seem to be affected by the severity of previous appendicitis, and prediction of recurrence is difficult to make based solely on inflammation severity.
Acknowledgements
The authors sincerely thank Shari Joy Berman for professionally editing the English draft of this manuscript.
Authors’ contributions
Study concept and design; YW and YT conceived the idea and developed the theory. Acquisition of data; YW, YK, and TO collected patient data. Data analysis and interpretation: YW, HJ, MN, and KA analyzed and interpreted the data. Drafting of the manuscripts; Yusuke Wakasa created the draft manuscript. Critical revision of the manuscript for important intellectual content; HK and YT discussed the results and contributed to the final version. Statistical analysis; YW performed the analytic calculations. Study supervision: YT and ME supervised the study. All the authors read and approved the manuscript.
Competing interests
The authors declare no conflict of interest for this study.
Funding
The authors did not receive any fund for this study.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon request.
Ethics approval and consent to participate
This study followed the World Medical Association Declaration of Helsinki and strengthening the reporting of observational studies in epidemiology (STROBE) guidelines for cohort studies. All procedures performed in studies involving human participants were in accordance with ethical standards; patient information was reviewed by the Institutional Ethical Review Board of Aomori City Hospital and informed consent exemption was obtained from the IRB of the affiliated institutions (Aomori City Hospital, Approval No. 2021 - 31). All experimental protocols were approved by the institutional committee (Aomori City Hospital, Approval No. 2021 - 31).
References
1. Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ. Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics. 2017;139(3):e20163003.
2. Minneci PC, Mahida JB, Lodwick DL, Sulkowski JP, Nacion KM, Cooper JN, et al. Effectiveness of patient choice in nonoperative vs surgical management of pediatric uncomplicated acute appendicitis. JAMA Surg. 2016;151(5):408-15.
3. Sallinen V, Akl EA, You JJ, Agarwal A, Shoucair S, Vandvik PO, et al. Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis. Br J Surg. 2016;103(6):656-667.
4. Huston JM, Kao LS, Chang PK, Sanders JM, Buckman S, Adams CA, et al. Antibiotics vs. appendectomy for acute uncomplicated appendicitis in adults: review of the evidence and future directions. Surg Infect (Larchmt). 2017;18(5):527-535.
5. Podda M, Gerardi C, Cillara N, Fearnhead N, CA Gomes 5, Arianna Birindelli 6, et al. Antibiotic treatment and appendectomy for uncomplicated acute appendicitis in adults and children: a systematic review and meta-analysis. Ann Surg. 2019;270(6):1028-1040.
6. Huang L, Yin Y, Yang L, Wang C, Li Y, Zhou Z. Comparison of antibiotic therapy and appendectomy for acute uncomplicated appendicitis in children. JAMA Pediatr. 2017;171(5):426-434.
7. Becker P, Fichtner-Feigl S, Schilling D. Clinical management of appendicitis. Visc Med. 2018;34(6):453-458.
8. Harnoss JC, Zelienka I, Probst P, Grummich K, Müller-Lantzsch C, Harnoss JM, et al. Antibiotics versus surgical therapy for uncomplicated appendicitis: systematic review and meta-analysis of controlled trials (PROSPERO 2015: CRD42015016882). Ann Surg. 2017;265(5):889-900.
9. Kasagi Y, Natsugoe K, Aoyagi T, Nobutou Y, Tsujita E, Ishida M, et al. Validating the efficacy of interval appendectomy for acute appendicitis: representative three cases with different etiologies. Surg Case Rep. 2020;6(1):207.
10. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-13.
11. Yamada T, Endo H, Hasegawa H, Kimura T, Kakeji Y, Koda K, et al. Risk of emergency surgery for complicated appendicitis: Japanese nationwide study. Ann Gastroenterol Surg. 2020;5(2):236-242.
12. Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246(5):741-8.
13. Yang Z, Sun F, Ai S, Wang J, Guan W, Liu S. Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 2019; 19(1):110.
14. Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377(9777): 1573-9.
15. Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg. 2006;244(5):656-60.
16. Hayes D, Reiter S, Hagen E, Lucas G, Chu I, Muñiz T, et al. Is interval appendectomy really needed? A closer look at neoplasm rates in adult patients undergoing interval appendectomy after complicated appendicitis. Surg Endosc. 2021;35(7):3855-3860.
17. Mällinen J, Rautio T, Grönroos J, Rantanen T, Nordström P, Savolainen H, et al. Risk of appendiceal neoplasm in periappendicular abscess in patients treated with interval appendectomy vs follow-up with magnetic resonance imaging. JAMA Surg. 2019;154(3):200-207.
18. Wright GP, Mater ME, Carroll JT, Choy JS, Chung MH. Is there truly an oncologic indication for interval appendectomy? Am J Surg. 2015;209(3):442-6.
19. Furman MJ, Cahan M, Cohen P, Lambert LA. Increased risk of mucinous neoplasm of the appendix in adults undergoing interval appendectomy. JAMA Surg. 2013;148(8):703-6.
20. Deelder JD, Richir MC, Schoorl T, Schreurs WH. How to treat an appendiceal inflammatory mass: operatively or nonoperatively? J Gastrointest Surg. 2014;18(4):641-5.
21. Carpenter SG, Chapital AB, Merritt MV, Johnson DJ. Increased risk of neoplasm in appendicitis treated with interval appendectomy: single-institution experience and literature review. Am Surg. 2012; 78(3):339-43.
22. Lee WS, Choi ST, Lee JN, Kim KK, Park YH, Baek JH. A retrospective clinicopathological analysis of appendiceal tumors from 3,744 appendectomies: a single-institution study. Int J Colorectal Dis. 2011;26(5):617-21.
23. Shindoh J, Niwa H, Kawai K, Ohata K, Ishihara Y, Takabayashi N, et al. Predictive factors for negative outcomes in initial nonoperative management of suspected appendicitis. J Gastrointest Surg. 2010; 14(2):309-14.
24. Kohga A, Kawabe A, Yajima K, Okumura T, Yamashita K, Isogaki J, et al. Does the presence of an appendicolith or abscess predict failure of nonoperative management of patients with acute appendicitis? Emerg Radiol. 2021;28(5):977-983.
25. Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82(2):166-9.
26. Hansson J, Körner U, Khorram-Manesh A, Solberg A, Lundholm K. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96(5):473-81.
27. Cobben LP, de Van Otterloo AM, Puylaert JB. Spontaneously resolving appendicitis: frequency and natural history in 60 patients. Radiology. 2000;215(2):349-52.
28. Liang TJ, Liu SI, Tsai CY, Kang CH, Huang WC, Chang HT, et al. Analysis of recurrence management in patients who underwent nonsurgical treatment for acute appendicitis. Medicine (Baltimore). 2016;95(12):e3159.
29. Chang YJ, Chao HC, Chen CL, Chen SY, Yan DC, Tsai MH. C-reactive protein may predict the recurrence of appendicitis in children formerly with appendiceal mass after successful nonoperative treatment. Pediatr Neonatol. 2017;58(4):350-354.
30. Ahmed I, Deakin D, Parsons S. Appendix mass: do we know how to treat it? Ann R Coll Surg Engl. 2005;87(3):191-5.
31 Oliak D, Yamini D, Udani VM, Lewis RJ, Arnell T, Vargas H, et al. Initial nonoperative management for periappendiceal abscess. Dis Colon Rectum. 2001;44(7):936-41.
32. Vanhatalo S, Munukka E, Sippola S, Jalkanen S, Grönroos J, Marttila H, et al. Prospective multicentre cohort trial on acute appendicitis and microbiota, aetiology and effects of antimicrobial treatment: study protocol for the MAPPAC (Microbiology APPendicitis ACuta) trial. BMJ Open. 2019;9(9):e031137.
33. Raahave D. Faecal retention: a common cause in functional bowel disorders, appendicitis, and haemorrhoids with medical and surgical therapy. Dan Med J. 2015;62(3):B5031.
34. Deli? J, Savkovi? A, Isakovi? E. Variations in the position and point of origin of the vermiform appendix. Med Arh. 2002;56(1):5-8. Croatian
Full Text Sources:
Abstract:
Views: 6368

For Authors
Journal Subscriptions

Jun 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News