Surgery, Gastroenterology and Oncology
Official journal of the International Association of Surgeons, Gastroenterologists and Oncologists
|
Primary Renal Non-Hodgkin Lymphoma: A Rare Case Report
CASE REPORT
ABSTRACT
Primary renal non-Hodgkin lymphoma is a rare extra-nodal lymphoma with a progressive characteristic and poor prognosis. We report on the case of a 73-year-old female with a painful right upper quadrant mass. The patient was planned for radical nephrectomy via laparotomy based on suspicion of renal cell carcinoma, shown on a urography CT scan. Intraoperatively, we identified a huge, solid, fixed mass originating from the right kidney; thus, a biopsy was performed. Histopathology and immunohistochemistry results showed a diffuse large B-cell lymphoma. Key words: primary renal lymphoma, DLBCL, biopsy laparotomy
INTRODUCTION
Although extra-nodal non-Hodgkin lymphoma commonly involves the kidney, with renal involvement seen in 30%?60% of cases (1), primary renal non- Hodgkin lymphoma (PRL) is rare, only occurring in 0.7%?1% of all extra-nodal lymphomas (2,3). PRL is localized to the kidney, without major lymph node disease (3,4). Symptoms, signs, and diagnostic examinations of PRL are atypical, causing PRL to be often misinterpreted as renal cell carcinoma (RCC) (4,5). Due to its scarcity, there is currently no consensus on optimal management or outcomes of this disease (6). In this case report, we present the clinical case of a 73-year-old female with a diagnosis of PRL.
CASE REPORT
A 73-year-old female presented with a chief complaint of a growing abdominal mass in the right upper quadrant for 4 months before hospital admission, with increasing pain over the previous 10 days.
 The patient experienced nausea and vomited several times, though there was no abdominal distention, changes in bowel habits, or reddish urine. The patient mentioned that she had lost 10 kg within the previous 4 months. She reported no masses in her neck or armpit regions.
The patient experienced nausea and vomited several times, though there was no abdominal distention, changes in bowel habits, or reddish urine. The patient mentioned that she had lost 10 kg within the previous 4 months. She reported no masses in her neck or armpit regions.
During the abdominal examination, we palpated a right upper quadrant mass that originated from the right kidney and had a size of 12 cm x 10 cm with solid consistency, uneven surface, and clear margins. The mass was fixed with distinct tenderness.
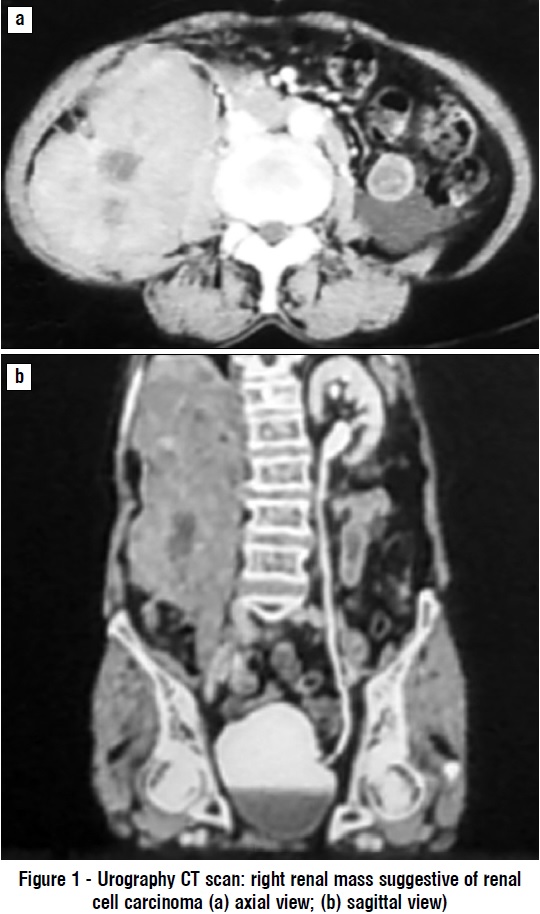
Laboratory examination showed normal complete blood count, blood chemistry, electrolyte levels, and urinalysis. A plain chest X-ray showed an elevated right diaphragm (suggestive of an intra-abdominal process) but found no sign of metastasis. Abdominal ultrasound indicated a right renal mass suggestive of RCC (differential diagnosis: urothelial tumor) with right hydronephrosis and found no metastasis to surrounding organs. Urography CT scan (fig. 1) visualized a right renal tumor suggestive of RCC.
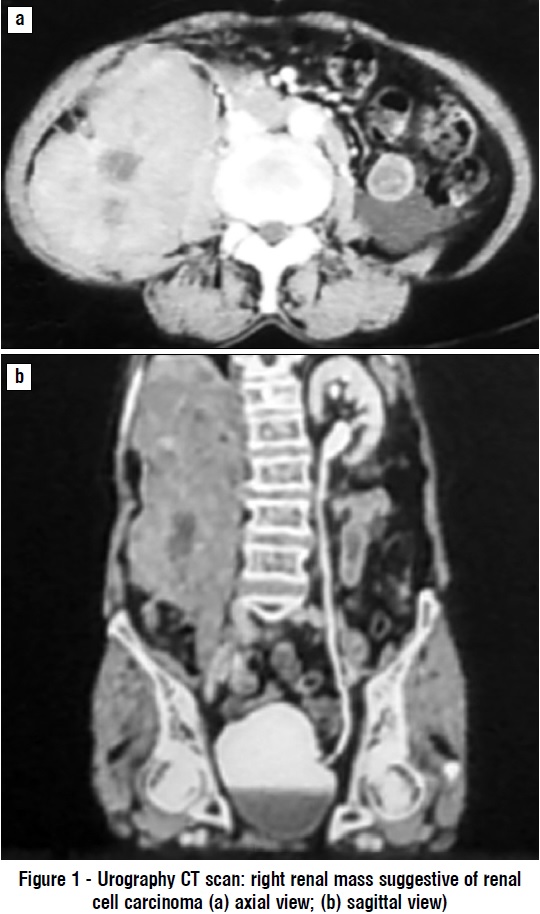
The patient was planned for a radical nephrectomy via laparotomy, but intraoperatively, we found that the tumor originated from the right kidney, was fixed to its surroundings with solid consistency, and caused diaphragm displacement upward. Based on these findings, we decided to perform a tumor biopsy. Histopathological examination (fig. 2) described malignant cell proliferation of small, round, blue tumor cells; further immunohistochemistry indicated diffuse large B-cell lymphoma (DLBCL) with positive CD45, CD20, BCL6, MUM1, and Ki-67. The patient died 4 months after being diagnosed.

DISCUSSION
This was the first PRL case in Makassar. In further research, we found no other cases of PRL in Indonesia. Vasquez-Alonso et al. mentioned that only 70 cases of PRL were recorded in the literature, with an incidence of 0.7% of all extra-nodal lymphomas (6). Chen et al reported that PRL accounted for 0.1% of all lymphomas in Japan (7).
According to the findings of Taneja et al, females made up 36.9% of PRL cases (4). Chen et al similarly reported that 37.1% of PRL cases occurred in females (2), indicating that PRL is more prevalent in the male population.
During the history taking, the patient complained of a painful abdominal mass for 4 months prior to admission and reported a 10-kg weight loss over the same period. Zhao et al and Chen et al conversely reported that patients with PRL demonstrated no typical signs and symptoms, such as flank pain, weight loss, hematuria, and giant renal mass (1,2).
The patient’s abdominal ultrasound showed a right renal mass suggestive of RCC (differential diagnosis: urothelial tumor) with right hydronephrosis. A urography CT scan also showed a right kidney mass suggestive of RCC. Zhao et al and Cheng et al concluded that PRL could be misinterpreted as RCC due to its scarcity; in their research, PRL tumors were described as homogenous masses with lower density, unclear margins, minimal vascularization, and less enhancement with contrast (1,8).
Tumor tissue, taken during laparotomy biopsy, was examined for histopathology and immunohistochemistry; the result indicated DLBCL, with positive CD45, CD20, BCL6, MUM1, and Ki-67. This DLBCL finding is globally the most common result for PRL (7). The primary therapy for PRL is chemotherapy with or without operation 5. This patient was scheduled to receive chemotherapy, though never initiated treatment due to her worsening condition.
This patient died 4 months after being diagnosed with PRL, illustrating the progressive characteristic of PRL, which was worsened by the lack of chemotherapy treatment. Bokhari et al described PRL as having a poor prognosis, even when it was not an extension of its primary disease (3). Cyriac et al and Vázquez-Alonso et al also identified the poor prognosis associated with PRL, reporting an average survival rate of < 1 year (6,9).
CONCLUSION
From the case described above, we can conclude that this was the first recorded case of PRL in Indonesia.
PRL has a progressive characteristic and a poor prognosis. The management of PRL is chemotherapy with or without operation. This case adds to the data on PRL and highlights the need for further research on this disease, particularly in Indonesia.
Conflict of interest:
The authors have stated that they have no conflicts of interest.
Ethical statement
The case report was done by following the ethical norms of scientific research and the principles anonymity a confidentiality.
REFERENCE
1. Zhao K, Zhang Q, Cong R, Wang Y, Wang Z, Song N. Primary renal lymphoma: a case report and review of the literature. AME Case Reports. 2020;4:8-8.
2. Chen J, Peng J, Zheng Y, Li S, Yang P, Wu X, et al. Primary renal lymphoma: a population-based study in the United States, 1980–2013. Sci Rep. 2019;9(1):1-10.
3. Bokhari SRA, Inayat F, Bokhari MR, Mansoor A. Primary renal lymphoma: A comprehensive review of the pathophysiology, clinical presentation, imaging features, management and prognosis. BMJ Case Rep. 2020;13(6).
4. Taneja A, Kumar V, Chandra AB. Primary renal lymphoma: A population- based analysis using the SEER program (1973-2015). Eur J Haematol. 2020;104(5):390-399.
5. Youssef M, Davis F, Rao P. Primary renal lymphoma: unique presentation in a rare disease. J Surg Case Reports. 2021;2021(3):1-3.
6. Vázquez-Alonso F, Puche-Sanz I, Sánchez-Ramos C, Flores-Martín J, Vicente-Prados J, Cózar-Olmo JM. Primary Renal Lymphoma: Long-Term Results of Two Patients Treated with a Chemotherapy + Rituximab Protocol. Case Rep Oncol Med. 2012;2012:1-3.
7. Chen X, Hu D, Fang L, Chen Y, Che X, Tao J, et al. Primary renal lymphoma: A case report and literature review. Oncol Lett. 2016; 12(5):4001-4008.
8. Cheng X, Huang Z, Li D, Wang Y. Enormous primary renal diffuse large B-cell lymphoma: A case report and literature review. J Int Med Res. 2019;47(6):2728-2739.
9. Cyriac S, Rejiv R, Shirley S, Sagar G. Primary renal lymphoma mimicking renal cell carcinoma. Indian J Urol. 2010;26(3):441.
Full Text Sources:
Abstract:
Views: 2071

ABSTRACT
Primary renal non-Hodgkin lymphoma is a rare extra-nodal lymphoma with a progressive characteristic and poor prognosis. We report on the case of a 73-year-old female with a painful right upper quadrant mass. The patient was planned for radical nephrectomy via laparotomy based on suspicion of renal cell carcinoma, shown on a urography CT scan. Intraoperatively, we identified a huge, solid, fixed mass originating from the right kidney; thus, a biopsy was performed. Histopathology and immunohistochemistry results showed a diffuse large B-cell lymphoma. Key words: primary renal lymphoma, DLBCL, biopsy laparotomy
INTRODUCTION
Although extra-nodal non-Hodgkin lymphoma commonly involves the kidney, with renal involvement seen in 30%?60% of cases (1), primary renal non- Hodgkin lymphoma (PRL) is rare, only occurring in 0.7%?1% of all extra-nodal lymphomas (2,3). PRL is localized to the kidney, without major lymph node disease (3,4). Symptoms, signs, and diagnostic examinations of PRL are atypical, causing PRL to be often misinterpreted as renal cell carcinoma (RCC) (4,5). Due to its scarcity, there is currently no consensus on optimal management or outcomes of this disease (6). In this case report, we present the clinical case of a 73-year-old female with a diagnosis of PRL.
CASE REPORT
A 73-year-old female presented with a chief complaint of a growing abdominal mass in the right upper quadrant for 4 months before hospital admission, with increasing pain over the previous 10 days.
 The patient experienced nausea and vomited several times, though there was no abdominal distention, changes in bowel habits, or reddish urine. The patient mentioned that she had lost 10 kg within the previous 4 months. She reported no masses in her neck or armpit regions.
The patient experienced nausea and vomited several times, though there was no abdominal distention, changes in bowel habits, or reddish urine. The patient mentioned that she had lost 10 kg within the previous 4 months. She reported no masses in her neck or armpit regions.During the abdominal examination, we palpated a right upper quadrant mass that originated from the right kidney and had a size of 12 cm x 10 cm with solid consistency, uneven surface, and clear margins. The mass was fixed with distinct tenderness.
Laboratory examination showed normal complete blood count, blood chemistry, electrolyte levels, and urinalysis. A plain chest X-ray showed an elevated right diaphragm (suggestive of an intra-abdominal process) but found no sign of metastasis. Abdominal ultrasound indicated a right renal mass suggestive of RCC (differential diagnosis: urothelial tumor) with right hydronephrosis and found no metastasis to surrounding organs. Urography CT scan (fig. 1) visualized a right renal tumor suggestive of RCC.
The patient was planned for a radical nephrectomy via laparotomy, but intraoperatively, we found that the tumor originated from the right kidney, was fixed to its surroundings with solid consistency, and caused diaphragm displacement upward. Based on these findings, we decided to perform a tumor biopsy. Histopathological examination (fig. 2) described malignant cell proliferation of small, round, blue tumor cells; further immunohistochemistry indicated diffuse large B-cell lymphoma (DLBCL) with positive CD45, CD20, BCL6, MUM1, and Ki-67. The patient died 4 months after being diagnosed.

DISCUSSION
This was the first PRL case in Makassar. In further research, we found no other cases of PRL in Indonesia. Vasquez-Alonso et al. mentioned that only 70 cases of PRL were recorded in the literature, with an incidence of 0.7% of all extra-nodal lymphomas (6). Chen et al reported that PRL accounted for 0.1% of all lymphomas in Japan (7).
According to the findings of Taneja et al, females made up 36.9% of PRL cases (4). Chen et al similarly reported that 37.1% of PRL cases occurred in females (2), indicating that PRL is more prevalent in the male population.
During the history taking, the patient complained of a painful abdominal mass for 4 months prior to admission and reported a 10-kg weight loss over the same period. Zhao et al and Chen et al conversely reported that patients with PRL demonstrated no typical signs and symptoms, such as flank pain, weight loss, hematuria, and giant renal mass (1,2).
The patient’s abdominal ultrasound showed a right renal mass suggestive of RCC (differential diagnosis: urothelial tumor) with right hydronephrosis. A urography CT scan also showed a right kidney mass suggestive of RCC. Zhao et al and Cheng et al concluded that PRL could be misinterpreted as RCC due to its scarcity; in their research, PRL tumors were described as homogenous masses with lower density, unclear margins, minimal vascularization, and less enhancement with contrast (1,8).
Tumor tissue, taken during laparotomy biopsy, was examined for histopathology and immunohistochemistry; the result indicated DLBCL, with positive CD45, CD20, BCL6, MUM1, and Ki-67. This DLBCL finding is globally the most common result for PRL (7). The primary therapy for PRL is chemotherapy with or without operation 5. This patient was scheduled to receive chemotherapy, though never initiated treatment due to her worsening condition.
This patient died 4 months after being diagnosed with PRL, illustrating the progressive characteristic of PRL, which was worsened by the lack of chemotherapy treatment. Bokhari et al described PRL as having a poor prognosis, even when it was not an extension of its primary disease (3). Cyriac et al and Vázquez-Alonso et al also identified the poor prognosis associated with PRL, reporting an average survival rate of < 1 year (6,9).
CONCLUSION
From the case described above, we can conclude that this was the first recorded case of PRL in Indonesia.
PRL has a progressive characteristic and a poor prognosis. The management of PRL is chemotherapy with or without operation. This case adds to the data on PRL and highlights the need for further research on this disease, particularly in Indonesia.
Conflict of interest:
The authors have stated that they have no conflicts of interest.
Ethical statement
The case report was done by following the ethical norms of scientific research and the principles anonymity a confidentiality.
REFERENCE
1. Zhao K, Zhang Q, Cong R, Wang Y, Wang Z, Song N. Primary renal lymphoma: a case report and review of the literature. AME Case Reports. 2020;4:8-8.
2. Chen J, Peng J, Zheng Y, Li S, Yang P, Wu X, et al. Primary renal lymphoma: a population-based study in the United States, 1980–2013. Sci Rep. 2019;9(1):1-10.
3. Bokhari SRA, Inayat F, Bokhari MR, Mansoor A. Primary renal lymphoma: A comprehensive review of the pathophysiology, clinical presentation, imaging features, management and prognosis. BMJ Case Rep. 2020;13(6).
4. Taneja A, Kumar V, Chandra AB. Primary renal lymphoma: A population- based analysis using the SEER program (1973-2015). Eur J Haematol. 2020;104(5):390-399.
5. Youssef M, Davis F, Rao P. Primary renal lymphoma: unique presentation in a rare disease. J Surg Case Reports. 2021;2021(3):1-3.
6. Vázquez-Alonso F, Puche-Sanz I, Sánchez-Ramos C, Flores-Martín J, Vicente-Prados J, Cózar-Olmo JM. Primary Renal Lymphoma: Long-Term Results of Two Patients Treated with a Chemotherapy + Rituximab Protocol. Case Rep Oncol Med. 2012;2012:1-3.
7. Chen X, Hu D, Fang L, Chen Y, Che X, Tao J, et al. Primary renal lymphoma: A case report and literature review. Oncol Lett. 2016; 12(5):4001-4008.
8. Cheng X, Huang Z, Li D, Wang Y. Enormous primary renal diffuse large B-cell lymphoma: A case report and literature review. J Int Med Res. 2019;47(6):2728-2739.
9. Cyriac S, Rejiv R, Shirley S, Sagar G. Primary renal lymphoma mimicking renal cell carcinoma. Indian J Urol. 2010;26(3):441.
Full Text Sources:
Abstract:
Views: 2071

Watch Video Articles
For Authors
Journal Subscriptions

Current Issue
Jun 2025
Supplements
Instructions for authors
Online submission
Contact
ISSN: 2559 - 723X (print)
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Open Access Statement
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Journal Metrics
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News