Surgery, Gastroenterology and Oncology
|
|
Background: There is a remaining high debate, about mesh fixation involved in laparoscopic inguinal hernia repair (LIHR) that is largely influenced by the individual preferences of each surgeon. In this research study, a comparison is done between mesh fixation in laparoscopic transabdominal preperitoneal (TAPP) using either staples or tissue adhesive (Amcrylate).
Methods: This was a prospective randomized controlled study that was applied to 100 patients having an inguinal hernia. Patients included were randomly sorted into two groups based on the closed envelope method; Group I, involved 50 patients previously subjected to laparoscopic TAPP, and tissue adhesive was used for mesh fixation, and GroupII, involved 50 patients subjected to laparoscopic TAPP, and tackers were used for fixation of mesh.
Results: We found a difference of statistical significance among the studied groups regarding the assessed VAS score on the 1st day (P=0.018), 10th day (P<0.001), and 30th days (P<0.001), post-operative with a difference that is not statistically significant pre-operative. The statistically analyzed difference among the studied groups was not significant regarding Carolina’s Comfort Scale after 6 months, Sensation of mesh, limitation of movement, recurrence, and complications.
Conclusion: Mesh fixation using tissue adhesive is preferable to staples because of its association with less post-surgery accompanied pain, earlier return to work, no increase in prompt recurrence rates and complications, better chronic pain experience, and comparable life quality.
INTRODUCTION
Inguinal hernia repair surgery is considered one of the most common worldwide surgeries as performed by more than 20 million patients annually (1). The classic method applied for inguinal hernia repair is the inguinal canal closure with the aid of sutures used. Regarding the high rate of recurrence of this approach, other methods were established involving synthetic meshes tensionfree implantation (2). Nowadays, endoscopic/laparoscopy approaches were performed for hernial repair. Two common laparoscopic methods are adopted transabdominal preperitoneal (TAPP) and extraperitoneal (TEP) repair (3). However, the debate is still going on about which of these approaches and methods is the best (4).
The mesh non-fixation is supposed to be the safest and least traumatic, but there have been multiple reports about the high mobility of the mesh, its low tensile strength, and elevated risk of recurrence if remained unfixed (5). In order to avoid the incidence of any dislocation of the mesh and in turn the hernial recurrence as well, variable fixation types have been suggested. On contrary to the penetrating fixation which is known for causing both acute and chronic pain, the adhesive fixation turned to be more popular with time as it decrease markedly both injury and chronic pain risk of incidence (6). Apart from the biological sealants as fibrin glue, surgical adhesives involve a group of synthetic glues and protein glues that are genetically engineered (7).
Multiple numbers of randomized trials have been observed with skepticism, as they have been identified as being underpowered for detecting the differences between LHR involving the use of tissue adhesives and mechanical fixation regarding chronic pain occurrence and recurrence prevalence (8). Accordingly, this study aimed to compare between fixation of mesh in laparoscopic TAPP using either staples or tissue adhesive (Amcrylate) as regards the following: detected Primary outcomes involving the rate of early recurrence and chronic pain occurrence, and Secondary Outcomes including complications and acute pain experienced postoperatively, the operating time and recovery to permit returning to work.
PATIENTS AND METHODS
This study was performed to be a randomized controlled study that was applied to cases admitted to Mansoura university hospital with inguinal hernia and fulfilled the eligibility criteria during the period from August 2019 to August 2021.
Sample size
Convenient sample of about 50 patients in each group, according to the flow rate of patients with inguinal hernia, were included due to limited time and resources of the study. The usual for our clinic to admit around 13 patients of inguinal every month. The duration of the study was 2 years from August 2019 to August 2021, we excluded the last 6 month of the study from operating new patients because they represent the least period needed for postoperative follow up period, also during the period from mars 2020 to august 2020 due to COVID-19 pandemic, elective surgery was suspended in our clinic and also there was a debate in laparoscopic procedure and relation to pandemic. Economic factor carries an impact also in our sample of operated patients. These factors affected the flow rate, hence the sample size was less than to be expected.
Inclusion criteria
All patients aged above 18 years old and fit for surgery considering the anesthesia by the American society of anesthesiologists (ASA) I & II.
Exclusion criteria
We excluded any patients with a recurrent hernia, complicated hernia, diabetic polyneuropathy, and spondyloarthritis or lumbar disc prolapse. In addition, any patients who had Contra indication to general anesthesia or pelvic laparoscopy were excluded. Written consent was taken from all patients after a good explanation of the procedure.
Randomization method
Patients were arbitrarily allocated into 2 groups; Group I, involved patients subjected to laparoscopic TAPP, and tissue adhesive was used for mesh fixation, Group II involved patients that were subjected to laparoscopic TAPP, and tackers were used for fixation of mesh. Simple randomization with 1:1 allocation ration has been done by means of online arbitatry generating package(www.randomization.com). Arbitrarily produced treatments have been put in closed envelop which was opened by the circulating nurse in the operating room and the patient was assigned to one of the two groups. This study was dual blinded as neither the patients nor the out come evaluators have knowledge about the grpoup to which the patient were allocated. The surgeons have knowledge about the study and group distribution.
Preoperative evaluation
Complete history taking, complete general examination, local examination to exclude complicated and recurrent hernia, routine lab investigation, anesthetic fitness assessment, and preoperative assessment of pain by visual analog scale (VAS) extends from 0 to 10, 0 means experiencing no pain and 10 means experiencing unbearable pain in between those 2 extremes, it is grading from mild to moderate to severe (9) fig. 1 as a basis for follow-up.

Intraoperative evaluation
As described by Bittner & Schwarz, 2012 (2). TAPP was done, the mesh which was used was Egymesh® it is microporous heavy weight polypropylene mesh available in Egypt.
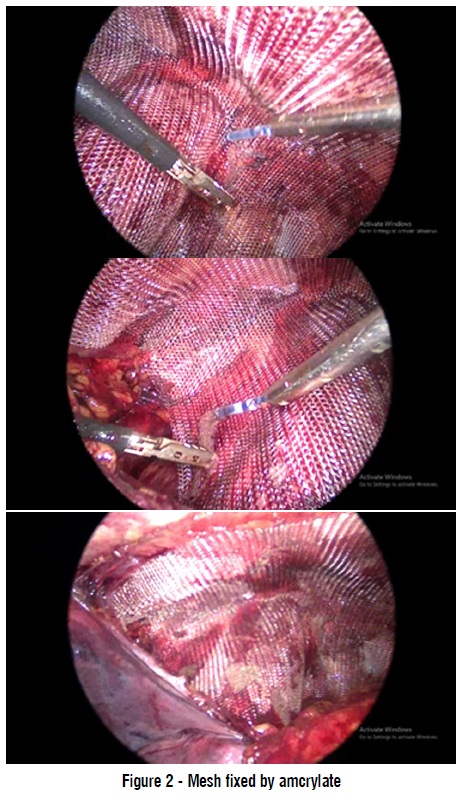
 mesh fixed by amcrylate
mesh fixed by amcrylate
During mesh fixation there were divided into two groups:
Group I: Tissue adhesive (Amcrylate®) was used for mesh fixation. The introduced glue application catheter was administered through a 5 mm trocar. An insulin syringe was adopted to ease the glue drop distribution. The tissue adhesive drops are situated on the mesh, that is kindly pressed against the underlying tissue whether above the symphysis pubis, the pubic arch medial of femoral vein, over the doomed triangle and pain triangle, at the superior iliac spine level, and both medial and lateral of the inferior vessels of epigastric. One or two ampules (.25 to .5 ml) were used for mesh fixation by getting more experience we were able to decrease the amount needed for mesh fixation (fig. 2).
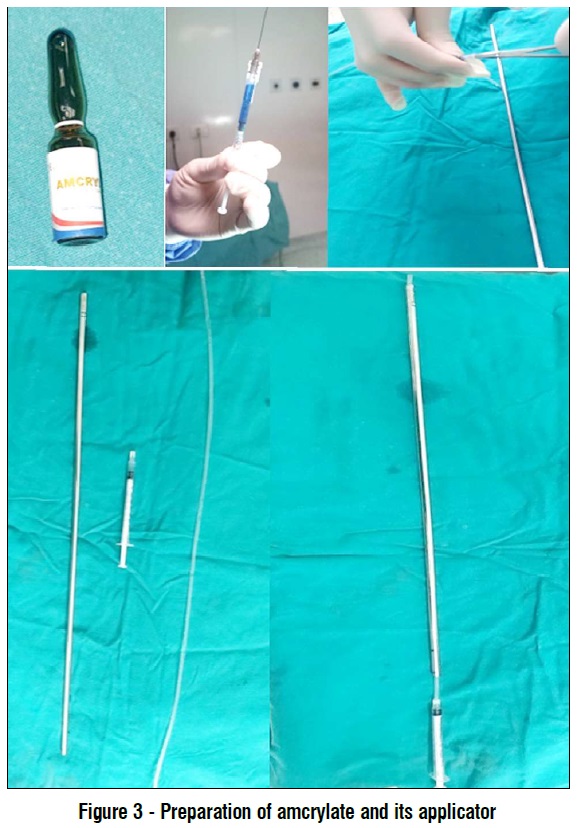
Amcrylate® is the trade name of cyanoacrylate which contain isoamyl chain, it has developed by Concord Drugs Limited. As long as it is dry, Amcrylate® remains inactive with no adhesive properties,but in the presence of water especially when it contains hydroxide ions like blood and other body fluids it become polymerized which gives him adhesive properties with the targeted surfaces. Adhesion between targeted surfaces starts within 5-6 seconds and become well developed in one minute. It has antibacterial properties. Time needed for elimination of the glue depend on quantity used. It disappear by hydrolytic break down after variable periods hydrolytic breakdown occurs (7).
As the applicator of the glue isn’t available in Egypt at the time of the study we passed by trials to reach a good and easy method of application. The applicator is formed by using outer sheath of previous tack or any similar instrument, the nelaton catheter 8 french is used and the insulin syringe nozzle is dilated to adapt the tip of the nelaton catheter (fig. 3).
Group II: Non-absorbable tackers (Bard®Capsure®) were used for the fixation of mesh. The first staple was applied at the ligament of cooper and then above the iliac spine level to prevent any lateral femoral cutaneous nerve injury occurrence. Followed by mesh fixation on the upper and medial edge, inversion of the pseudosac by tack to decrease the dead space (fig. 4).
Bard®Capsure® is non-absorbable spiral tack 5 mm thickness formed of 316L stainless steel and covered by polyetheretherketone-PEEK smooth cap to provide atraumatic and smooth surface facing the abdomen. It is spiral provide easy penetration and high peel strength (10).
Finally, closure of peritoneum by stitches Vicryl 2/0, closure of camera port, and skin closure were done. Operative time was recorded starting from the time of skin incision until the closure.
Post-operative
A fixed dose of analgesia as parenteral NSAIDS for the first-day post-operative followed by paracetamol fixed dose for first-week post-operative. Post-operative pain by VAS on day 1, day 10, and day 30 postoperative by VAS.

Time taken for returning to work was calculated. Postoperative experienced chronic pain was evaluated by using a CCS questionnaire (table 1) (11) within 6 months postoperative. The CCS was created and licensed by the Gastrointestinal and Minimally Invasive Surgery Division of Carolinas Medical Centre located in Charlotte, NC. Postoperative complications either related to the method of fixation or not were recorded. Follow up for prescence of recurrence was done either by patient complain at any time or direct examination 6 months postoperative.

Statistical analysis and interpretation of data
Data were introduced in the computer to be analyzed using IBM SPSS Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. Qualitative data were expressed in the form of calculated numbers and percentages. Quantitative data were represented after calculating the mean, and the standard deviation after undergoing normality testing through the Kolmogorov-Smirnov test in the case of normally distributed data. The obtained results’ significance was evaluated in reference to the (0.05) level. For qualitative data type, the chi-Square test and the Monte Carlo test were both used to compare 2 or more groups. For comparing a quantitative data type among groups, a student t-test was performed inorder to compare 2 independent groups.
RESULTS
Group I mean age is 38.14 years versus 40 years among group II. In both groups, males were more predominant than females. The difference detected among the studied groups is of no statistical significance regarding their age and sex. The operative mean time for group I is 77.9 minutes versus 74.82 minutes for group II with no reported statistically significant difference (table 2).
We have classified the hernia in size and location according to European Hernia Society(EHS) groin hernia classification and finding were non-significant difference between both groups (table 3).

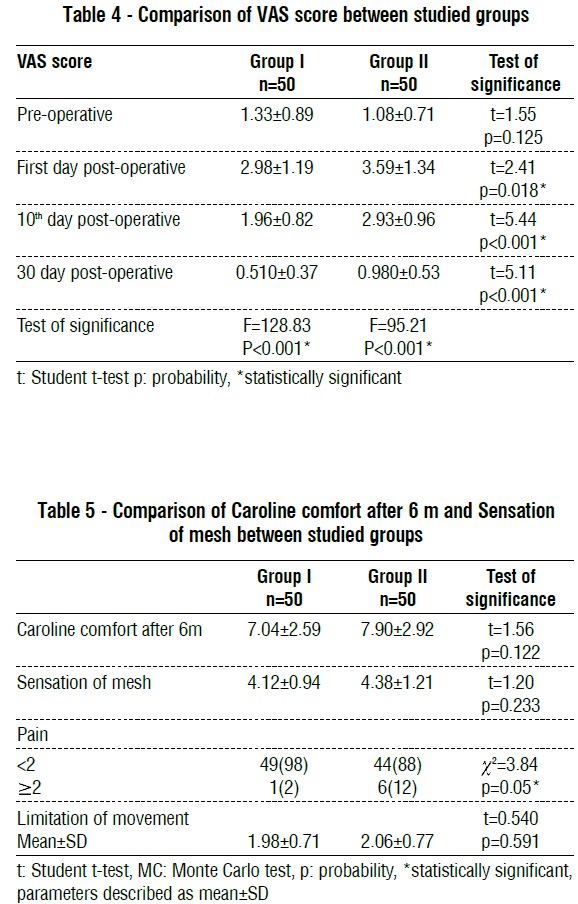
VAS scores among groups are demonstrated in (table 4). The VAS mean score was higher for group II than group I post-operative. In each group, the highest mean VAS score was reported on the 1st following day postoperative, while the lowest score was reported on the 30th day postoperative. We found that the detected postoperative difference among the studied groups was significant regarding the statistically analyzed VAS score on the first day (P=0.018), 10th day (P<0.001), and 30th days (P<0.001), and exhibiting no pre-operative statistically significant difference. Also, there is the difference that is statistically significant in each group among both the preoperative and postoperative indicated VAS scores (on 1st, 10th, and 30th days) (P<0.001, for both).
Table 5 demonstrates a difference in statistical significance among the groups involved in the study regarding chronic pain (P=0.05) with one case with chronic pain included in group I versus 6 cases involved in group II. No difference of statistical significance between the study groups regarding Caroline’s comfort after 6 months, Sensation of mesh, and limitation of movement.
The mean return to work time among group II was significantly higher than group I (9.64 versus 7.96 days, respectively, P<0.001). Intraoperative complications were not detected among both study groups. There was a difference that was non-statistically significant between the studied groups regarding the recurrence incidence and the complications with one case of recurrence detected for group I and one for group II. Seroma is detected among 10% of group I versus 4% for group II and one case of hematoma for group II (table 6).
Cases of recurrence in each group were readmitted and managed by Lichtenstein tension-free open mesh repair. All cases of seroma were managed conservatively except for 1 case in group I that required repeated tapping resolved within 2 months. Hematoma in 1 patient in group II and no cases in group I, the patient was readmitted to the hospital and investigated for the source of ecchymosis but nothing could be detected and it was managed conservatively.
DISCUSSION
Fixation of mesh in LIHR is still highly debated, being probably influenced by the individual preferences of each surgeon (3). Our study aimed to perform a comparison between mesh fixation in laparoscopic TAPP using either staples or tissue adhesive (Amcrylate).
According to operative time in our study, the difference detected is not significant statistically among the studied groups considering the operation time with a mean operative time being 77.9 minutes for group I versus 74.82 minutes for group II. Our findings are consistent with those of Shi, et al (12) and Burza et al (13).
We can notice that operative time is variable between studies as it depends on many factors like the surgical experience of the operator, patient hernia classification, method of mesh fixation and peritoneum closure, type of mesh, and its liability for easy handling and manipulation. In our study for both groups, we used microporous heavy-weight polypropylene mesh, and dealing with this mesh not so easy especially as regard its memory, and the peritoneum was sutured by vicryl 2/0 the difference was in mesh fixation. Using tissue adhesive at fixation has consumed more time, especially at the first few cases till we reached a good method for application. In our study, we assessed perioperative pain by using VAS, preoperatively, there was no statistically significant difference between the two groups. Postoperative there was increase in pain for the the first day postoperativly with overall improvement of pain over the time. There was a difference of statistical significance among the studied groups on the first day, 10th day and 30 days with less pain in group I.
Wang, et al (14) compared adhesive fixation by cyanoacrylate versus titanium spiral tacks there was a difference that was significant statistically between both involved groups as regarded by VAS score in firstday postoperative favoring non-mechanical fixation. On the other side, Fortelny et al (15) and Li et al (16) showed no significant difference between both groups according to acute postoperative pain.

Effects of methods of fixation on postoperative pain have been documented but it is not wise to assume that it is the only variant that affects post-operative pain at the early post-operative stages. According to Sharma et al (17) many factors influence postoperative accompanied acute pain like preventive analgesia, the used port type, ports size, hernia sac complete reduction vs the proximally involved ligation and transection, usage of transversus abdominis block, the material of mesh used, and mesh size and fixation approach, local anesthesia instillation in a dissected space, both skin and port sites closure. All previously discussed items were fixed for all paients in our study.
According to Brokelman, et al (18) the pain assessment is considered difficult as a result of being a multifaceted expression of affection, cognition and also physical, sensory, behavioral, social-cultural, and subjective related feelings.
In our study, we have assessed the post-operative return to work taken period, we ask the involved patients to return to their normal activity and work that doesn’t require strenuous physical activity, it shows a statistically significant difference with a higher mean return to work time among group II than group I (9.64 versus 7.96 days, respectively).
Lovisetto et al (19) showed that with concerning both groups of TAPP by mesh fixation using Tissucol fibrin glue versus staples. A significantly faster return to normal activities was detected among the glue group when compared with the involved staples group (one returned after 7.9 days vs. the other one returned after 9.1 days, respectively ).
On the other side, Brügger et al (20) detected a difference of no statistical significance between both involved study groups regarding the return to normal activity, this copes with regarding post-operative pain no significant difference was noticed.
We can detect that early return to work was associated with the improvement in acute postoperative pain. In the presence of statistically significant improvement of acute postoperative pain in favor of tissue adhesive, it wasn’t unexpected to find a return to work is more early with statistical significance in favor of group used tissue adhesive.
Recurrence was the classic and the most important point when we deal with surgical repair of the hernia. Displacement of the mesh from its position which covers all sites of hernia at the myopectineal orifice is considered the main concern when we deal with causes of early recurrence. In our study, the statistically determined difference found among the studied groups was not significant regarding the recurrence probability of incidence with one case of recurrence detected for each group. In group I, the patient who showed recurrence was detected 3 weeks postoperative, and this patient developed chest problems and attacks of severe cough started 10 days postoperative which may explain the early recurrence, while in group II the recurrence was detected 10 weeks postoperative and there was no apparent cause for recurrence. As detected in our study Li, et al (16), Brügger et al (20) and Antoniou, et al (8) comparing recurrence in non-penetrating as tissue adhesive versus mechanical fixation of mesh in LIHR has showed no difference between the studied groups of these different studies.
In our study, a difference that was non-statistically significant among the studied groups regarding complication incidence, Seroma was detected among 10% of group I versus 4% for group II and 1 case of hematoma for group II. During mechanical fixation in group II we have used tacking and inversion of the pseudo sac of fascia transversalis to decrease dead space with higher incidence of direct hernia in group I and cyanoacrylate my show local tissue reaction increase seroma formation this explain higher incidence of seroma in group I. The mesh used is micro porous heavyweight polypropylene mesh is also associated with high incidence of seroma. Hematoma can occur more with group II due to possibility of injury by penetration.
Similar to our study Brügger, et al (20) and Shah et al (21) the difference was insignificant between both involved groups either tacks or fibrin glue, but fibrin glue is associated with more seroma formation.
In contrast, Olmi, et al (22) showed that seroma and hematoma were significantly less in the fibrin group than with tackers. Tolver et al (23) showed nosignificant difference as regards seroma or hematoma and both were higher in the tacks group.
In our study we used CCS to assess the quality of life, so we added more parameters, not just pain but also the limitation of movement and sensation of mesh were added and there was a quality of life enhancement in favor of the study group of non-mechanical fixation, but the difference wasn’t statistically significant between both involved study groups.
The determined difference involved in our study was statistically significant among the studied groups in relation to chronic pain with one case among group I versus 6 cases among group II, we defined chronic pain as when patient gives a score more than 1 at sensation of pain at any item at the CCS which means it is bothering the patient.
Antoniou et al (8) showed a reported chronic pain that accounts for about 6.2% and 11.8% of total patients subjected to a performed repair using bio glue or mechanical fixation, respectively. The postoperative pain sensed persists for more than 3 months long and increases with penetrating mesh fixation. Wang et al (14) detected no chronic pain in non-fixation and cyanoacrylate with 2.2% in cases of staple fixation and 2.1 % in cyanoacrylate plus Staple. Brügger et al (20) exhibited a lower chronic pain incidence among the tissue adhesive study group than in the tacks group, but it wasn’t statistically significant. A chronic pain metaanalysis from the five RCTs showed the statistical significance of non-mechanical fixation experience less pain (21).
We can notice that non-mechanical fixation is associated within studies with less chronic pain whether it is significant or not. However, the sample size may be associated with different interpretations for different results as for the large size of sample leads to statistically significant even minute details (24).
Cost represents an important factor when we deal with multiple choices for managing certain diseases especially when we are taking into our mind that results are comparable between both methods and with points of improvement as regards the use of tissue adhesive (amcrylate ) which was used in our study for unilateral hernia 1 – 2 ampoules is sufficient for mesh fixation at our chosen points and this provides good fixation after our first cases in the study when we have managed to reach our good application method usually one ampoule was sufficient the cost of one ampoule at the start our study was available for 200 Egyptian pounds and reached for 250 Egyptian pounds around 12 USD on the other side tacker was available for 6000 Egyptian pounds and reached 10000 around 450 USD thousand at end of our study, so as a direct cost of amcrylate, it is far away less than tacks. Cost and economic points may need better assessment for many factors that contribute to the total cost either direct or indirect.
Limitations included Relatively small sample size who were collected from a single surgical center and flow rate was affected by COVID-19 pandemic. Also, our study lacks follow up for a long term.
CONCLUSION
Laparoscopic TAPP repair for inguinal hernias is indicated for inguinal hernias because it is a safe method that allows for early recovery and less morbidity. Mesh fixation using tissue adhesive is preferable to staples due to its relation with lower postsurgery pain, quick return to work, no increase in rapid recurrence rate or complications, better chronic pain experience and quality of life was comparable.
Conflict of interest
All author declare that they have no conflict of interest.
Ethical approval
For performing this study ethical approval was obtained.
REFERENCES
1. Köckerling F, Simons MP. Current Concepts of Inguinal Hernia Repair. Visceral medicine. 2018;34(2):145-50.
2. Bittner R, Schwarz J. Inguinal hernia repair: current surgical techniques. Langenbeck's archives of surgery. 2012;397(2):271-82.
3. Habib Bedwani NAR, Kelada M, Smart N, Szydlo R, Patten DK, Bhargava A. Glue versus mechanical mesh fixation in laparoscopic inguinal hernia repair: meta-analysis and trial sequential analysis of randomized clinical trials. Br J Surg. 2021;108(1):14-23.
4. Arregui M. Chain of Events Leading to the Development of the Current Techniques of Laparoscopic Inguinal Hernia Repair: The Time Was Ripe. In: Bittner R, Köckerling F, Fitzgibbons JRJ, LeBlanc KA, Mittal SK, Chowbey P, editors. Laparo-endoscopic Hernia Surgery: Evidence Based Clinical Practice. Berlin, Heidelberg: Springer Berlin Heidelberg; 2018. p. 31-5.
5. Kumar A, Kaistha S, Gangavatiker R. Non-fixation Versus Fixation of Mesh in Totally Extraperitoneal Repair of Inguinal Hernia: a Comparative Study. Indian J Surg. 2018;80(2):128-133.
6. Birk D, Hess S, Garcia-Pardo C. Low recurrence rate and low chronic pain associated with inguinal hernia repair by laparoscopic placement of Parietex ProGrip™ mesh: clinical outcomes of 220 hernias with mean follow-up at 23 months. Hernia. 2013;17(3):313-20.
7. Kukleta JF, Freytag C, Weber M. Efficiency and safety of mesh fixation in laparoscopic inguinal hernia repair using n-butyl cyanoacrylate: long-term biocompatibility in over 1,300 mesh fixations. Hernia. 2012;16(2):153-62.
8. Antoniou SA, Köhler G, Antoniou GA, Muysoms FE, Pointner R, Granderath FA. Meta-analysis of randomized trials comparing nonpenetrating vs mechanical mesh fixation in laparoscopic inguinal hernia repair. Am J Surg. 2016;211(1):239-249.e2.
9. Lazaridou A, Elbaridi N, Edwards RR, Berde CB. Chapter 5 - Pain Assessment. In: Benzon HT, Raja SN, Liu SS, Fishman SM, Cohen SP, editors. Essentials of Pain Medicine (Fourth Edition): Elsevier; 2018. p. 39-46.e1.
10. Kapoulas S, Papalois A, Papadakis G, Tsoulfas G, Christoforidis E, Papaziogas B, et al. Safety and efficacy of absorbable and nonabsorbable fixation systems for intraperitoneal mesh fixation: an experimental study in swine. Hernia. 2022;26(2):567-579.
11. Parseliunas A, Paskauskas S, Simatoniene V, Vaitekunas J, Venskutonis D. Adaptation and validation of the Carolinas Comfort Scale: a questionnaire-based cross-sectional study. Hernia. 2022; 26(3):735-744.
12. Shi Z, Fan X, Zhai S, Zhong X, Huang D. Fibrin glue versus staple for mesh fixation in laparoscopic transabdominal preperitoneal repair of inguinal hernia: a meta-analysis and systematic review. Surg Endosc. 2017;31(2):527-537.
13. Burza A, Avantifiori R, Curinga R, Santini E, Delle Site P, Stipa F. Comparison between two different mesh fixation methods in laparoscopic inguinal hernia repair: tacker vs. Synthetic cyanoacrylate glue. Minerva chirurgica. 2014;69(6):321-9. Italian
14. Wang MG, Tian ML, Zhao XF, Nie YS, Chen J, Shen YM. Effectiveness and safety of n-butyl-2-cyanoacrylate medical adhesive for noninvasive patch fixation in laparoscopic inguinal hernia repair. Surg Endosc. 2013;27(10):3792-8.
15. Fortelny RH, Petter-Puchner AH, May C, Jaksch W, Benesch T, Khakpour Z, et al. The impact of atraumatic fibrin sealant vs. staple mesh fixation in TAPP hernia repair on chronic pain and quality of life: results of a randomized controlled study. Surg Endosc. 2012; 26(1):249-54.
16. Li J, Ji Z, Zhang W. Staple Fixation Against Adhesive Fixation in Laparoscopic Inguinal Hernia Repair: A Meta-Analysis of Randomized Controlled Trials. Surg Laparosc Endosc Percutan Tech. 2015;25(6):471-7.
17. Sharma N, Sharma D, Meena S. Minimizing Pain in Laparoscopic Hernia Surgery. In: Sharma D, Hazrah P, editors. Recent Concepts in Minimal Access Surgery: Volume 1. Singapore: Springer Singapore; 2022. p. 283-91.
18. Brokelman RB, Haverkamp D, van Loon C, Hol A, van Kampen A, Veth R. The validation of the visual analogue scale for patient satisfaction after total hip arthroplasty. Eur Orthop Traumatol. 2012; 3(2):101-105.
19. Lovisetto F, Zonta S, Rota E, Mazzilli M, Bardone M, Bottero L, et al Use of human fibrin glue (Tissucol) versus staples for mesh fixation in laparoscopic transabdominal preperitoneal hernioplasty: a prospective, randomized study. Ann Surg. 2007;245(2):222-31.
20. Brügger L, Bloesch M, Ipaktchi R, Kurmann A, Candinas D, Beldi G. Objective hypoesthesia and pain after transabdominal preperitoneal hernioplasty: a prospective, randomized study comparing tissue adhesive versus spiral tacks. Surg Endosc. 2012;26(4):1079-85.
21. Shah NS, Fullwood C, Siriwardena AK, Sheen AJ. Mesh fixation at laparoscopic inguinal hernia repair: a meta-analysis comparing tissue glue and tack fixation. World J Surg. 2014;38(10):2558-70.
22. Olmi S, Scaini A, Erba L, Bertolini A, Croce E. Laparoscopic repair of inguinal hernias using an intraperitoneal onlay mesh technique and a Parietex composite mesh fixed with fibrin glue (Tissucol). Personal technique and preliminary results. Surg Endosc. 2007;21(11): 1961-4.
23. Tolver MA, Rosenberg J, Juul P, Bisgaard T. Randomized clinical trial of fibrin glue versus tacked fixation in laparoscopic groin hernia repair. Surg Endosc. 2013;27(8):2727-33.
24. Heniford BT, Lincourt AE, Walters AL, Colavita PD, Belyansky I, Kercher KW, et al. Carolinas Comfort Scale as a Measure of Hernia Repair Quality of Life: A Reappraisal Utilizing 3788 International Patients. Ann Surg. 2018;267(1):171-176.
Full Text Sources:
Abstract:
Views: 3181

For Authors
Journal Subscriptions

Jun 2025
Supplements
Instructions for authors
Online submission
Contact
e-ISSN: 2601 - 1700 (online)
ISSN-L: 2559 - 723X
Journal Abbreviation: Surg. Gastroenterol. Oncol.
Surgery, Gastroenterology and Oncology (SGO) is indexed in:
- SCOPUS
- EBSCO
- DOI/Crossref
- Google Scholar
- SCImago
- Harvard Library
- Open Academic Journals Index (OAJI)
Surgery, Gastroenterology and Oncology (SGO) is an open-access, peer-reviewed online journal published by Celsius Publishing House. The journal allows readers to read, download, copy, distribute, print, search, or link to the full text of its articles.
Time to first editorial decision: 25 days
Rejection rate: 61%
CiteScore: 0.2

Meetings and Courses in 2025
Meetings and Courses in 2024
Meetings and Courses in 2023
Meetings and Courses in 2022
Meetings and Courses in 2021
Meetings and Courses in 2020
Meetings and Courses in 2019
Verona expert meeting 2019

Surgery, Gastroenterology and Oncology applies the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits readers to copy and redistribute the material in any medium or format, remix, adapt, build upon the published works non-commercially, and license the derivative works on different terms, provided the original material is properly cited and the use is non-commercial. Please see: https://creativecommons.org/licenses/by-nc/4.0/
Publisher’s Note:
The opinions, statements, and data contained in article are solely those of the authors and not of Surgery, Gastroenterology and Oncology journal or the editors. Publisher and the editors disclaim responsibility for any damage resulting from any ideas, instructions, methods, or products referred to in the content.
 IASGO Society News
IASGO Society News